7 november 2024: zie ook dit artikel: https://kanker-actueel.nl/galwegstents-via-de-buikwand-en-haip-intra-arteriele-chemotherapie-voorkomen-minder-complicaties-en-verlengen-overall-overleving-bij-patienten-met-gevorderde-en-inoperabele-galwegenkanker.html
4 mei 2017: Bron: Journal of Clinical Oncology
Inmiddels is het studierapport van de Nederlandse oncoloog Bart Groot Koerkamp online gepubliceerd in het Journal of Clinical Oncology.
Het volledige studierapport: Perioperative Hepatic Arterial Infusion Pump Chemotherapy Is Associated With Longer Survival After Resection of Colorectal Liver Metastases: A Propensity Score Analysis is gratis in te zien. Het blijft heel raar dat ondanks alle bewijzen dat HAIPO voortreffeljke resultaten laat zien dat in Nederland / Europa nog een nieuwe gerandomiseerde placebo gecontroleerde fase III studie moet plaatsvinden. Met dus als uitkomst dat zeker tientallen mensen met in de lever uitgezaaide darmkanker onnodig vroegtijdig zullen overlijden.Ik vraag me af of we wellicht in samenwerking met patiënten organisaties hiertegen actie moeten ondernemen? Ik ga het in ieder geval voorleggen aan mijn collega's patient advocates binnen Inspire2live. (Tekst gaat verder onder grafiek)
Het abstract staat onderaan dit artikel.
21 april 2017: Bron: AD en J Gastrointest Oncology
Het Algemeen Dagblad komt vandaag 21 april 2017 met een ervaringsverhaal van een Nederlandse man, Cas Renders die al in 2000 met HAIP - hepatic arterial infusion pump therapy is behandeld in het Memorial Sloan Kettering in New York voor zijn in de lever uitgezaaide darmkanker en in 2000 nog slechts een levensverwachting van drie maanden kreeg. En met succes want hij is 17 jaar later (hij is nu 54 jaar) nog steeds kankervrij. Een mooi ervaringsverhaal maar de manier van behandelen wordt al heel lang toegepast in Amerika.
HAIP - hepatic arterial infusion pump therapy is al een oude techniek die vooral in Amerika veel wordt toegepast. Vooral bij primaire leverkanker maar ook bij operabele in de lever uitgezaaide darmkanker. In feite is dit TACE - chemo embolisatie zoals ook dr. Vogl die toepast maar omdat het pompje in de lever wordt geplaatst bij de operatieve verwijdering van de tumoren kan deze chemo embolisatie zonder extra belasting voor de patiënt om de twee weken worden uitgevoerd.
Bekijk deze video hoe HAIP wordt uitgevoerd: Treating Liver Metastases with Hepatic Arterial Infusion Therapy
Een uitstekende review studie over HAIP - hepatic arterial infusion pump therapy is deze studie: Hepatic resection, hepatic arterial infusion pump therapy, and genetic biomarkers in the management of hepatic metastases from colorectal cancer
In this review, we discuss surgical treatment and associated outcomes in the treatment of CRLM. In addition, the role and efficacy of HAI therapy are examined. Finally, we outline how genetic profiling and mutational analysis can impact management of this disease in this era of molecular-based targeted therapies. Abstract sataat hieronder met referentielijst.
Chirurg-oncoloog Bas Groot Koerkamp deed onderzoek naar de resultaten van HAIP bij 2000 Amerikaanse patienten en uit zijn onderzoek blijkt dat mediaan de patienten 2 jaar langer leefden dan alleen met systemische chemo. Maar blijkbaar is dit bewijs niet voldoende om dit aan Nederlandse en Belgische patienten aan te bieden want er komt nu eerst een gerandomiseerde placebo gecontroleerde fase III studie. Het is toch van de gekke dat na zoveel bewijs (google op HAIP - hepatic arterial infusion pump therapy en u vindt tientallen studies) er weer opnieuw een studie moet worden gedaan. Trots wordt in het artikel in het AD vermeldt dat het KWF deze studie financiert. Wat een verspilling van tijd en geld ten koste van kankerpatiënten, wetende dat deze manier van behandelen spotgoedkoop is in vergelijking met de nieuwere medicijnen en dat er nog weer een placebo gecontroleerde fase III studie mee moet worden gedaan. SCHANDALIG
Hier een citaat uit het artikel in het Algemeen Dagblad d.d. 21 april 2017
Langer leven dankzij simpel chemopompje
Mensen met darmkanker en uitzaaiingen in de lever kunnen spectaculair langer leven door een speciale chemopomp. Dat blijkt uit onderzoek van het Erasmus MC onder Amerikaanse patiënten. Het apparaat komt nu naar Nederland.........
Cas Renders (54) uit Amsterdam is het levende bewijs. In 2000 – op zijn 38ste – gaven artsen hem 4 procent kans om te overleven ,,Of wel: over 3 maanden bent u er niet meer.” Hij gaf niet op en kwam bij kankercentrum Sloan Kettering in New York terecht.
Daar plaatsen ze het pompje ter grootte van een ijshockeypuck net onder zijn huid en spuiten er om de twee weken chemovloeistof in, zes keer in totaal. Groot Koerkamp: ,,De pomp zit op de slagader en voert direct chemo de lever in. Omdat het ook alleen dáár blijft, kun je een heel hoge concentratie gebruiken.” Bijkomend voordeel: de patiënt heeft nauwelijks last van bijwerkingen die horen bij chemokuren via een infuus, zoals misselijkheid en haarverlies. Lees het volledige artikel in het AD>>>>>>>>>>
Het volledige studierapport Hepatic resection, hepatic arterial infusion pump therapy, and genetic biomarkers in the management of hepatic metastases from colorectal cancer is gratis in te zien.
Hier het abstract met referentielijst
HAI chemotherapy has also evolved, and provides a unique and effective therapy both in the unresectable setting and as an adjuvant therapy following resection seemingly beyond that of systemic therapies alone.
Hepatic resection, hepatic arterial infusion pump therapy, and genetic biomarkers in the management of hepatic metastases from colorectal cancer
Use of perioperative hepatic arterial infusion pump chemotherapy after complete resection of colorectal liver metastases is associated with a marked improvement in overall survival compared with systemic chemotherapy without hepatic arterial infusion
DOI: 10.1200/JCO.2016.71.8346 Journal of Clinical Oncology - published online before print April 20, 2017
Perioperative Hepatic Arterial Infusion Pump Chemotherapy Is Associated With Longer Survival After Resection of Colorectal Liver Metastases: A Propensity Score Analysis
Bas Groot Koerkamp, Eran Sadot, Nancy E. Kemeny, Mithat Gönen, Julie N. Leal, Peter J. Allen, Andrea Cercek, Ronald P. DeMatteo, T. Peter Kingham, William R. Jarnagin, and Michael I. D’Angelica
Bas Groot Koerkamp, Eran Sadot, Nancy E. Kemeny, Mithat Gönen, Julie N. Leal, Peter J. Allen, Andrea Cercek, Ronald P. DeMatteo, T. Peter Kingham, William R. Jarnagin, and Michael I. D’Angelica, Memorial Sloan Kettering Cancer Center, New York, NY; Bas Groot Koerkamp, Erasmus MC Cancer Institute, Rotterdam, the Netherlands; and Eran Sadot, Rabin Medical Center, Petah Tikva, and Tel Aviv University, Tel Aviv, Israel.
To investigate whether perioperative hepatic arterial infusion pump chemotherapy (HAI) was associated with overall survival (OS) in patients who had a complete resection of colorectal liver metastases (CLM).
Patients who underwent a complete resection of CLM between 1992 and 2012 were included from a single-center prospectively maintained database. All patients who received HAI also received perioperative systemic chemotherapy. Propensity score analysis was used to match patients for seven known prognostic factors.
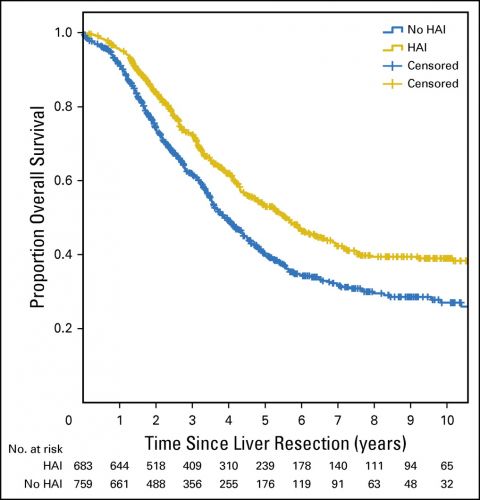
A total of 2,368 consecutive patients underwent a complete resection of CLM, with a median follow-up of 55 months. The median OS for patients with HAI (n = 785) was 67 months versus 44 months without HAI (n = 1,583; P < .001), despite more advanced disease in the HAI group. OS at 10 years was 38.0% versus 23.8% without HAI. For patients who received modern systemic chemotherapy (n = 1,442), the median OS was 67 months with HAI and 47 months without HAI (P < .001). The hazard ratio adjusted by propensity score demonstrated longer OS with HAI: 0.67 (95% CI, 0.59 to 0.76; P < .001). A pronounced difference in median OS was found for patients with node-negative colorectal cancer (129 months with HAI v 51 months without; P < .001) and a low clinical risk score of 0 to 2 points (89 months with HAI v 53 months without; P < .001).
Patients who received HAI had a median OS of approximately 2 years longer than patients without HAI. The strong association was independent of the use of modern systemic chemotherapy and remained in propensity score analysis. Patients with node-negative primary tumors or a low clinical risk score seemed to benefit most from HAI.
| 1. | Siegel R, Ma J, Zou Z, et al: Cancer statistics, 2014. CA Cancer J Clin 64:9-29, 2014 CrossRef, Medline |
| 2. | Tomlinson JS, Jarnagin WR, DeMatteo RP, et al: Actual 10-year survival after resection of colorectal liver metastases defines cure. J Clin Oncol 25:4575-4580, 2007 Link |
| 3. | Nordlinger B, Sorbye H, Glimelius B, et al: Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): Long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14:1208-1215, 2013 CrossRef, Medline |
| 4. | Portier G, Elias D, Bouche O, et al: Multicenter randomized trial of adjuvant fluorouracil and folinic acid compared with surgery alone after resection of colorectal liver metastases: FFCD ACHBTH AURC 9002 trial. J Clin Oncol 24:4976-4982, 2006 Link |
| 5. | de Jong MC, Pulitano C, Ribero D, et al: Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: An international multi-institutional analysis of 1669 patients. Ann Surg 250:440-448, 2009 Medline |
| 6. | Ackerman NB: The blood supply of experimental liver metastases. IV. Changes in vascularity with increasing tumor growth. Surgery 75:589-596, 1974 Medline |
| 7. | Ensminger WD, Gyves JW: Clinical pharmacology of hepatic arterial chemotherapy. Semin Oncol 10:176-182, 1983 Medline |
| 8. | Kemeny N, Huang Y, Cohen AM, et al: Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med 341:2039-2048, 1999 CrossRef, Medline |
| 9. | Kemeny NE, Gonen M: Hepatic arterial infusion after liver resection. N Engl J Med 352:734-735, 2005 CrossRef, Medline |
| 10. | Kemeny MM, Adak S, Gray B, et al: Combined-modality treatment for resectable metastatic colorectal carcinoma to the liver: surgical resection of hepatic metastases in combination with continuous infusion of chemotherapy--an intergroup study. J Clin Oncol 20:1499-1505, 2002 Medline |
| 11. | Lorenz M, Müller HH, Schramm H, et al: Randomized trial of surgery versus surgery followed by adjuvant hepatic arterial infusion with 5-fluorouracil and folinic acid for liver metastases of colorectal cancer. Ann Surg 228:756-762, 1998 CrossRef, Medline |
| 12. | DʼAngelica MI, Correa-Gallego C, Paty PB, et al: Phase II trial of hepatic artery infusional and systemic chemotherapy for patients with unresectable hepatic metastases from colorectal cancer: Conversion to resection and long-term outcomes. Ann Surg 261:353-360, 2015 CrossRef, Medline |
| 13. | Kemeny N, Capanu M, D’Angelica M, et al: Phase I trial of adjuvant hepatic arterial infusion (HAI) with floxuridine (FUDR) and dexamethasone plus systemic oxaliplatin, 5-fluorouracil and leucovorin in patients with resected liver metastases from colorectal cancer. Ann Oncol 20:1236-1241, 2009 |
| 14. | Kemeny N, Jarnagin W, Paty P, et al: Phase I trial of systemic oxaliplatin combination chemotherapy with hepatic arterial infusion in patients with unresectable liver metastases from colorectal cancer. J Clin Oncol 23:4888-4896, 2005 Link |
| 15. | Kemeny NE, Melendez FD, Capanu M, et al: Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma. J Clin Oncol 27:3465-3471, 2009 Link |
| 16. | Kemeny NE, Niedzwiecki D, Hollis DR, et al: Hepatic arterial infusion versus systemic therapy for hepatic metastases from colorectal cancer: A randomized trial of efficacy, quality of life, and molecular markers (CALGB 9481). J Clin Oncol 24:1395-1403, 2006 Link |
| 17. | Edge S, Byrd DR, Compton CC, et al: AJCC Cancer Staging Manual (ed 7). New York, NY, Springer, 2010 |
| 18. | Fong Y, Fortner J, Sun RL, et al: Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: Analysis of 1001 consecutive cases. Ann Surg 230:309-318, 1999; discussion 318-321 |
| 19. | Bennett JJ, Schmidt CR, Klimstra DS, et al: Perihepatic lymph node micrometastases impact outcome after partial hepatectomy for colorectal metastases. Ann Surg Oncol 15:1130-1136, 2008 CrossRef, Medline |
| 20. | Cardona K, Donataccio D, Kingham TP, et al: Treatment of extensive metastatic colorectal cancer to the liver with systemic and hepatic arterial infusion chemotherapy and two-stage hepatic resection: The role of salvage therapy for recurrent disease. Ann Surg Oncol 21:815-821, 2014 CrossRef, Medline |
| 21. | Robins JM, Mark SD, Newey WK: Estimating exposure effects by modelling the expectation of exposure conditional on confounders. Biometrics 48:479-495, 1992 CrossRef, Medline |
| 22. | Kalbfleisch JD, Prentice RL: The Statistical Analysis of Failure Time Data (ed 2). Hoboken, NJ, Wiley-Interscience, 2002 |
| 23. | House MG, Kemeny NE, Gönen M, et al: Comparison of adjuvant systemic chemotherapy with or without hepatic arterial infusional chemotherapy after hepatic resection for metastatic colorectal cancer. Ann Surg 254:851-856, 2011 CrossRef, Medline |
| 24. | Hamady ZZ, Lodge JP, Welsh FK, et al: One-millimeter cancer-free margin is curative for colorectal liver metastases: A propensity score case-match approach. Ann Surg 259:543-548, 2014 CrossRef, Medline |
| 25. | Deschamps F, Rao P, Teriitehau C, et al: Percutaneous femoral implantation of an arterial port catheter for intraarterial chemotherapy: Feasibility and predictive factors of long-term functionality. J Vasc Interv Radiol 21:1681-1688, 2010 CrossRef, Medline |
| 26. | Goéré D, Benhaim L, Bonnet S, et al: Adjuvant chemotherapy after resection of colorectal liver metastases in patients at high risk of hepatic recurrence: A comparative study between hepatic arterial infusion of oxaliplatin and modern systemic chemotherapy. Ann Surg 257:114-120, 2013 CrossRef, Medline |
| 27. | Allen PJ, Nissan A, Picon AI, et al: Technical complications and durability of hepatic artery infusion pumps for unresectable colorectal liver metastases: An institutional experience of 544 consecutive cases. J Am Coll Surg 201:57-65, 2005 CrossRef, Medline |
| 28. | Ito K, Ito H, Kemeny NE, et al: Biliary sclerosis after hepatic arterial infusion pump chemotherapy for patients with colorectal cancer liver metastasis: Incidence, clinical features, and risk factors. Ann Surg Oncol 19:1609-1617, 2012 CrossRef, Medline |
| 29. | Moulton CA, Gu CS, Law CH, et al: Effect of PET before liver resection on surgical management for colorectal adenocarcinoma metastases: A randomized clinical trial. JAMA 311:1863-1869, 2014 CrossRef, Medline |
Plaats een reactie ...
2 Reacties op "HAIP -(hepatic arterial infusion pump), chemo embolisatie via in lever geplaatste pomp verlengt leven van patienten met darmkamker met uitzaaiingen in de lever mediaan met 2 jaar."
Gerelateerde artikelen
- HAIP -(hepatic arterial infusion pump), chemo embolisatie via in lever geplaatste pomp verlengt leven van patienten met darmkamker met uitzaaiingen in de lever mediaan met 2 jaar.
- Arteriele chemo embolisatie geeft significant veel betere resultaten op overleving, progressie vrije tijd en kwaliteit van leven dan systemische chemo bij patienten met darmkanker met uitzaaiingen in de lever copy 1
- TACE = Transarteriële Chemo Embolisatie: Veel informatie en studieresultaten bij elkaar gezet in 1 artikelenreeks, waar ook informatie is te lezen over LITT - Laser Institial Tumor Therapy




Ik heb uitgezaaide leverkanker zeer kwaad aardig
Ik ben momenteel met mijn derde chemotherapie bezig.
Imuumtherapie helpt niet.
Graag wil ik informatie over waar ik zo'n pomp kan krijgen hier in Nederland of Amerika
Hoor erg graag van u
Groet Esther
Of bij dr. Bas Groot Koerkamp zelf: https://www.erasmusmc.nl/chirurgieErasmusMC/Transplantatiechirurgie/BehandelteamTransplantatieChirurgie/WieisuwTransplantatiechirurg/b-groot-koerkamp/
U zou dan het Erasmus zelf moeten bellen en laten doorverbinden met dr. Groot Koerkamp: 010) 704 0 704
Laat u ons wat weten mocht het gelukt zijn?
Kees braam
webmaster www.kanker-actueel.nl