Mocht u kanker-actueel de moeite waard vinden en ons willen ondersteunen om kanker-actueel online te houden dan kunt u ons machtigen voor een periodieke donatie via donaties: https://kanker-actueel.nl/NL/donaties.html of doneer al of niet anoniem op - rekeningnummer NL79 RABO 0372931138 t.n.v. Stichting Gezondheid Actueel in Amersfoort. Onze IBANcode is NL79 RABO 0372 9311 38
Elk bedrag is welkom. En we zijn een ANBI instelling dus uw donatie of gift is in principe aftrekbaar voor de belasting. En als donateur kunt u ook korting krijgen bij verschillende bedrijven:
https://kanker-actueel.nl/NL/voordelen-van-ops-lidmaatschap-op-een-rijtje-gezet-inclusief-hoe-het-kookboek-en-de-recepten-op-basis-van-uitgangspunten-van-houtsmullerdieet-te-downloaden-enof-in-te-zien.html
8 september 2015: zie ook dit artikel:
kurkuma-curcumine-supplementen-beschermt-vrouwen-met-borstkanker-tegen-huidschade-dermatitis-door-bestraling-met-60-procent-verschil-copy-1
8 september 2015: bron: Br J Radiol. June 2014; 87(1038): 20130490. Published online 2014 May 5. doi: 10.1259/bjr.20130490
Een zalf met sandelhoutolie en tumeric - curcuma erin voorkomt veel beter dermatitis - huidschade door bestraling dan babyolie bij patiënten met hoofd-halstumoren (mond- en keelkanker) die daarvoor werden bestraald. Het verschil van graad 3 optredende dermatitis bedroeg ca. 75% in effectiviteit: 9.5% kreeg graad 3 dermatitis in de curcuma bevattende zalfgroep versus 37.5% voor de babyolie groep (p < 0.01).
Ook duurde het langer voordat patiënten die de curcuma bevattende zalf gebruikten voor er een huidbeschadiging optrad dan bij de babyolie. En in het studierapport wordt melding gemaakt dat wanneer bij de patiënten uit de babyoliegroep dermatitis optrad de curcuma bevattende zalf dit nog gedeeltelijk herstelde.
Hier een fotoreeks van gradatie van dermatitis:

Ik heb al eerder gezegd dat ik levertraanzalf gebruikte tijdens de bestraling met goede resultaten. En zie ook het artikel in gerelateerde artikelen over curcuma suppletie bij borstkankerpatiënten die bestraald werden met enorme verschillen in dermatitis die optrad door de bestraling.
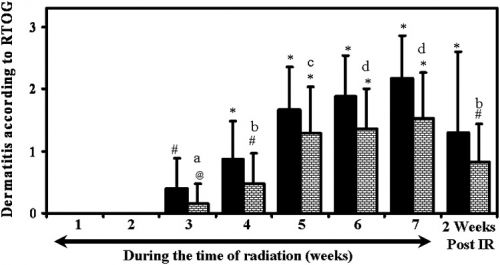
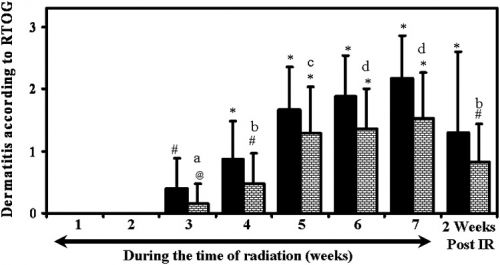
Hier de resultaten in een grafiek weergegeven bij de patiënten met hoofd- halstumoren:
Het volledige studierapport: Topical application of a sandal wood oil and turmeric based cream prevents radiodermatitis in head and neck cancer patients undergoing external beam radiotherapy: a pilot study is gratis in te zien, dus ik vertaal maar niet alles.
Deze studie is uitgevoerd door een bedrijf dat de door hun zelf ontwikkelde en gebruikte zalf als merknaam uitvent, maar het lijkt mij dat een andere zalf die curcuma en sandelhoutolie bevat waarschijnlijk hetzelfde effect zal geven. Het is zo ergelijk dat aan fabrikanten gevraagd wordt om dit soort studies tegen heel veel geld te moeten laten uitvoeren. terwijl gebruikersstudies met geen merknaam maar wel met de ingredienten zoveel sneller resultaat op zou kunnen leveren.
Hier het abstract van de studie:
VTC - Vicco® turmeric cream is shown to be effective in preventing radiodermatitis
Br J Radiol. June 2014; 87(1038): 20130490.
Topical application of a sandal wood oil and turmeric based cream prevents radiodermatitis in head and neck cancer patients undergoing external beam radiotherapy: a pilot study
P L Palatty, MB BS, MD,
1 A Azmidah, MB BS,
2 S Rao, MB BS, MD,
3,* D Jayachander, MB BS, MD,
3 K R Thilakchand, MB BS,
2 M P Rai, MB BS,
2,* R Haniadka, MB BS,
2 P Simon, MB BS,
2 R Ravi, MB BS,
2 R Jimmy, MB BS,
2,* P F D'souza, MB BS,
2 R Fayad, MB BS, MD,
4 and
M S Baliga, MSc, PhD
 2
2
Abstract
Objective:
The study objective was to assess the effectiveness of a turmeric- and sandal wood oil-containing cream [Vicco® turmeric cream (VTC); Vicco Laboratories, Parel, India] on radiodermatitis in patients with head and neck cancer undergoing radiotherapy.
Methods:
A total of 50 patients with head and neck cancer requiring >60 Gy of curative radiotherapy/chemoradiotherapy were enrolled in the study. The volunteers were randomly divided into two groups of 25 patients. Group 1 was assigned to a topical application of Johnson's® baby oil (Johnson & Johnson Ltd, Baddi, India) and Group 2 for VTC. Prophylactic application of the cream was initiated on Day 1 and continued every day until 2 weeks after the end of treatment. Both agents were symmetrically applied within the irradiated field five times a day, and the acute skin reactions were assessed twice weekly in accordance with the Radiation Therapy Oncology Group scores by an investigator who was unaware of the details.
Results:
The incidence of radiodermatitis increased with the exposure to radiation and was the highest in both groups at Week 7. However, a significant reduction in grades of dermatitis were seen in cohorts applying VTC at all time points, including 2 weeks post radiotherapy (p < 0.015 to p < 0.001). The occurrence of Grade 3 dermatitis was lower in the cohorts using VTC and was statistically significant (p < 0.01). Additionally, follow-up observations 2 weeks after the completion of radiotherapy also showed a reduced degree of radiodermatitis in cohorts applying VTC, which was significant (p = 0.015).
Conclusion:
VTC is shown to be effective in preventing radiodermatitis and needs to be validated in larger double-blind trials.
Advances in knowledge:
For the first time, this study shows that the turmeric- and sandal oil-based cream was effective in preventing radiation-induced dermatitis.
REFERENCES
1.
Baskar R, Lee KA, Yeo R, Yeoh KW. Cancer and radiation therapy: current advances and future directions. Int J Med Sci 2012; 9: 193–9. doi: 10.7150/ijms.3635 [PMC free article] [PubMed] [Cross Ref]2.
Uma Devi P. Normal tissue protection in cancer therapy—progress and prospects. Acta Oncol 1998; 37: 247–52. [PubMed]3.
Ryan JL. Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol 2012; 132: 985–93. doi: 10.1038/jid.2011.411 [PMC free article] [PubMed] [Cross Ref]4.
McQuestion M. Evidence-based skin care management in radiation therapy. Semin Oncol Nurs 2006; 22: 163–73. doi: 10.1016/j.soncn.2006.04.004 [PubMed] [Cross Ref]5.
Bolderston A, Lloyd NS, Wong RK, Holden L, Robb-Blenderman L; Supportive Care Guidelines Group of Cancer Care Ontario Program in Evidence-Based Care. The prevention and management of acute skin reactions related to radiation therapy: a systematic review and practice guideline. Support Care Cancer 2006; 14: 802–17. doi: 10.1007/s00520-006-0063-4 [PubMed] [Cross Ref]6.
Salvo N, Barnes E, van Draanen J, Stacey E, Mitera G, Breen D, et al. . Prophylaxis and management of acute radiation-induced skin reactions: a systematic review of the literature. Curr Oncol 2010; 17: 94–112. [PMC free article] [PubMed]7.
Naylor W, Mallett J. Management of acute radiotherapy induced skin reactions: a literature review. Eur J Oncol Nurs 2001; 5: 221–3. [PubMed]8.
Noble-Adams R. Radiation-induced reactions 1: an examination of the phenomenon. Br J Nurs 1999; 8: 1134–40. [PubMed]9. Glean E, Edwards S, Faithfull S, Meredith C, Richards C, Smith M, et al. . Intervention for acute radiotherapy induced skin reactions in cancer patients: the development of a clinical guideline recommended for use by the college of radiographers. J Radiother Pract 2001; 2: 75–84.
10.
Radvansky LJ, Pace MB, Siddiqui A. Prevention and management of radiation-induced dermatitis, mucositis, and xerostomia. Am J Health Syst Pharm 2013; 70: 1025–32. doi: 10.2146/ajhp120467 [PubMed] [Cross Ref]11.
Weiss JF, Landauer MR. Protection against ionizing radiation by antioxidant nutrients and phytochemicals. Toxicology 2003; 189: 1–20. [PubMed]12.
Fang YZ, Yang S, Wu G. Free radicals, antioxidants, and nutrition. Nutrition 2002; 18: 872–9. [PubMed]13.
Muller K, Meineke V. Radiation-induced alterations in cytokine production by skin cells. Exp Hematol 2007; 35: 96–104. [PubMed]14.
Hymes SR, Strom EA, Fife C. Radiation dermatitis: clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol 2006; 54: 28–46. doi: 10.1016/j.jaad.2005.08.054 [PubMed] [Cross Ref]15.
Olsen DL, Raub W Jr, Bradley C, Johnson M, Macias JL, Love V, et al. . The effect of aloe vera gel/mild soap versus mild soap alone in preventing skin reactions in patients undergoing radiation therapy. Oncol Nurs Forum 2001; 28: 543–7. [PubMed]16.
Heggie S, Bryant GP, Tripcony L, Keller J, Rose P, Glendenning M, et al. . A phase III study on the efficacy of topical aloe vera gel on irradiated breast tissue. Cancer Nurs 2002; 25: 442–51. [PubMed]17.
Becker-Schiebe M, Mengs U, Schaefer M, Bulitta M, Hoffmann W. Topical use of a silymarin-based preparation to prevent radiodermatitis: results of a prospective study in breast cancer patients. Strahlenther Onkol 2011; 187: 485–91. [PubMed]18.
Pommier P, Gomez F, Sunyach MP, D'Hombres A, Carrie C, Montbarbon X. Phase III randomized trial of Calendula officinalis compared with trolamine for the prevention of acute dermatitis during irradiation for breast cancer. J Clin Oncol 2004; 22: 1447–53. [PubMed]19. Baliga MS, Venkatesh S, Mrinal S, Bala N, Palatty PL. Turmeric (Curcuma longa L) the Indian golden curry spice as a skin care agent: validation of the traditional uses. In: Waston RR, Zibadi S, editor. , eds. Bioactive dietary factors and plant extracts in dermatology. New York, NY: Humana Press; 2013. pp. 93–102.
20.
Kundu S, Biswas TK, Das P, Kumar S, De DK. Turmeric (Curcuma longa) rhizome paste and honey show similar wound healing potential: a preclinical study in rabbits. Int J Low Extrem Wounds 2005; 4: 205–13. doi: 10.1177/1534734605281674 [PubMed] [Cross Ref]21. Khare P, Khare S, Goswami RB, Pathak AK. Evaluation of comparative effect of intact plant formulation & its polyherbal formulation for wound healing activity. Plant Archives 2010; 10: 671–4.
22.
Srimal RC, Dhawan BN. Pharmacology of diferuloyl methane (curcumin), a non-steroidal anti-inflammatory agent. J Pharm Pharmacol 1973; 25: 447–52. [PubMed]23.
Sidhu GS, Singh AK, Thaloor D, Banaudha KK, Patnaik GK, Srimal RC, et al. . Enhancement of wound healing by curcumin in animals. Wound Repair Regen 1998; 6: 167–77. [PubMed]24.
Gopinath D, Ahmed MR, Gomathi K, Chitra K, Sehgal PK, Jayakumar R. Dermal wound healing processes with curcumin incorporated collagen films. Biomaterials 2004; 25: 1911–17. [PubMed]25.
Singer AJ, McClain SA, Romanov A, Rooney J, Zimmerman T. Curcumin reduces burn progression in rats. Acad Emerg Med 2007; 14: 1125–9. doi: 10.1197/j.aem.2007.07.012 [PubMed] [Cross Ref]26.
Sajithlal GB, Chithra P, Chandrakasan G. Effect of curcumin on the advanced glycation and cross-linking of collagen in diabetic rats. Biochem Pharmacol 1998; 56: 1607–14. [PubMed]27.
Mani H, Sidhu GS, Kumari R, Gaddipati JP, Seth P, Maheshwari RK. Curcumin differentially regulates TGF-beta1, its receptors and nitric oxide synthase during impaired wound healing. Biofactors 2002; 16: 29–43. [PubMed]28.
López-Jornet P, Camacho-Alonso F, Jiménez-Torres MJ, Orduña-Domingo A, Gómez-García F. Topical curcumin for the healing of carbon dioxide laser skin wounds in mice. Photomed Laser Surg 2011; 29: 809–14. [PubMed]29.
Singer AJ, Taira BR, Lin F, Lim T, Anderson R, McClain SA, et al. . Curcumin reduces injury progression in a rat comb burn model. J Burn Care Res 2011; 32: 135–42. doi: 10.1097/BCR.0b013e318203337b [PubMed] [Cross Ref]30.
Kulac M, Aktas C, Tulubas F, Uygur R, Kanter M, Erboga M, et al. . The effects of topical treatment with curcumin on burn wound healing in rats. J Mol Histol 2013; 44: 83–90. doi: 10.1007/s10735-012-9452-9 [PubMed] [Cross Ref]31.
Phan TT, See P, Lee ST, Chan SY. Protective effects of curcumin against oxidative damage on skin cells in vitro: its implication for wound healing. J Trauma 2001; 51: 927–31. [PubMed]32.
Lima CF, Pereira-Wilson C, Rattan SI. Curcumin induces heme oxygenase-1 in normal human skin fibroblasts through redox signaling: relevance for anti-aging intervention. Mol Nutr Food Res 2011; 55: 430–42. doi: .10.1002/mnfr.201000221 [PubMed] [Cross Ref]33.
Heng MC, Song MK, Harker J, Heng MK. Drug-induced suppression of phosphorylase kinase activity correlates with resolution of psoriasis as assessed by clinical, histological and immunohistochemical parameters. Br J Dermatol 2000; 143: 937–49. [PubMed]34.
Pol A, Bergers M, Schalkwijk J. Comparison of antiproliferative effects of experimental and established antipsoriatic drugs on human keratinocytes, using a simple 96-well-plate assay. In Vitro Cell Dev Biol Anim 2003; 39: 36–42. [PubMed]35.
Saelee C, Thongrakard V, Tencomnao T. Effects of Thai medicinal herb extracts with anti-psoriatic activity on the expression on NF-κB signaling biomarkers in HaCaT keratinocytes. Molecules 2011; 16: 3908–32. [PubMed]36.
Sumiyoshi M, Kimura Y. Effects of a turmeric extract (Curcuma longa) on chronic ultraviolet B irradiation-induced skin damage in melanin-possessing hairless mice. Phytomedicine 2009; 16: 1137–43. doi: 10.1016/j.phymed.2009.06.003 [PubMed] [Cross Ref]37.
Agrawal R, Kaur IP. Inhibitory effect of encapsulated curcumin on ultraviolet-induced photoaging in mice. Rejuvenation Res 2010; 13: 397–410. doi: 10.1089/rej.2009.0906 [PubMed] [Cross Ref]38.
Lu YP, Chang RL, Huang MT, Conney AH. Inhibitory effect of curcumin on 12-O-tetradecanoylphorbol-13-acetate-induced increase in ornithine decarboxylase mRNA in mouse epidermis. Carcinogenesis 1993; 14: 293–7. [PubMed]39.
Cho JW, Park K, Kweon GR, Jang BC, Baek WK, Suh MH, et al. . Curcumin inhibits the expression of COX-2 in UVB-irradiated human keratinocytes (HaCaT) by inhibiting activation of AP-1: p38 MAP kinase and JNK as potential upstream targets. Exp Mol Med 2005; 37: 186–92. doi: 10.1038/emm.2005.25 [PubMed] [Cross Ref]40.
Asawanonda P, Klahan SO. Tetrahydrocurcuminoid cream plus targeted narrowband UVB phototherapy for vitiligo: a preliminary randomized controlled study. Photomed Laser Surg 2010; 28: 679–84. doi: 10.1089/pho.2009.2637 [PubMed] [Cross Ref]41.
Azuine MA, Bhide SV. Chemopreventive effect of turmeric against stomach and skin tumors induced by chemical carcinogens in Swiss mice. Nutr Cancer 1992; 17: 77–83. doi: 10.1080/01635589209514174 [PubMed] [Cross Ref]42.
Villaseñor IM, Simon MK, Villanueva AM. Comparative potencies of nutraceuticals in chemically induced skin tumor prevention. Nutr Cancer 2002; 44: 66–70. [PubMed]43.
Limtrakul P, Lipigorngoson S, Namwong O, Apisariyakul A, Dunn FW. Inhibitory effect of dietary curcumin on skin carcinogenesis in mice. Cancer Lett 1997; 24: 197–203. [PubMed]44.
Limtrakul P, Anuchapreeda S, Lipigorngoson S, Dunn FW. Inhibition of carcinogen induced c-Ha-ras and c-fos proto-oncogenes expression by dietary curcumin. BMC Cancer 2001; 1: 1. [PMC free article] [PubMed]45.
Huang MT, Smart RC, Wong CQ, Conney AH. Inhibitory effect of curcumin, chlorogenic acid, caffeic acid, and ferulic acid on tumor promotion in mouse skin by 12-O-tetradecanoylphorbol-13-acetate. Cancer Res 1988; 48: 5941–6. [PubMed]46.
Huang MT, Newmark HL, Frenkel K. Inhibitory effects of curcumin on tumorigenesis in mice. J Cell Biochem Suppl 1997; 27: 26–34. [PubMed]47.
Kuttan R, Sudheeran PC, Josph CD. Turmeric and curcumin as topical agents in cancer therapy. Tumori 1987; 73: 29–31. [PubMed]48.
Ryan JL, Heckler CE, Ling M, Katz A, Williams JP, Pentland AP, et al. . Curcumin for radiation dermatitis: a randomized, double-blind, placebo-controlled clinical trial of thirty breast cancer patients. Radiat Res 2013; 180: 34–43. [PMC free article] [PubMed]49.
Dwivedi C, Abu-Ghazaleh A. Chemopreventive effects of sandal wood oil on skin papillomas in mice. Eur J Cancer Prev 1997; 6: 399–401. [PubMed]50.
Dwivedi C, Guan X, Harmsen WL, Voss AL, Goetz-Parten DE, Koopman EM, et al. . Chemopreventive effects of alpha-santalol on skin tumor development in CD-1 and SENCAR mice. Cancer Epidemiol Biomarkers Prev 2003; 12: 151–6. [PubMed]51.
Dwivedi C, Maydew ER, Hora JJ, Ramaeker DM, Guan X. Chemopreventive effects of various concentrations of alpha-santalol on skin cancer development in CD-1 mice. Eur J Cancer Prev 2005; 14: 473–6. [PubMed]52.
Dwivedi C, Valluri HB, Guan X, Agarwal R. Chemopreventive effects of alpha-santalol on ultraviolet B radiation-induced skin tumor development in SKH-1 hairless mice. Carcinogenesis 2006; 27: 1917–22. doi: 10.1093/carcin/bgl058 [PubMed] [Cross Ref]53.
Bommareddy A, Hora J, Cornish B, Dwivedi C. Chemoprevention by alpha-santalol on UVB radiation-induced skin tumor development in mice. Anticancer Res 2007; 27: 2185–8. [PubMed]54.
Santha S, Dwivedi C. α-Santalol, a skin cancer chemopreventive agent with potential to target various pathways involved in photocarcinogenesis. Photochem Photobiol 2013; 89: 919–26. doi: .10.1111/php.12070 [PubMed] [Cross Ref]55. Pazdur R, Wagman L, Camphausen K, Hoskins WJ, editor. , eds. Cancer management: a multidisciplinary approach. 12th edn. Norwalk, CT: CMP Healthcare Media LLC; 2009.
56.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995; 31: 1341–6. doi: 10.1016/0360-3016(95)00060-C [PubMed] [Cross Ref]57.
Noble-Adams R. Radiation-induced reactions 2: development of a measurement tool. Br J Nurs 1999; 8: 1208–11. [PubMed]58.
Thangapazham RL, Sharma A, Maheshwari RK. Beneficial role of curcumin in skin diseases. Adv Exp Med Biol 2007; 595: 343–57. doi: 10.1007/978-0-387-46401-5_15 [PubMed] [Cross Ref]59.
Thangapazham RL, Sharad S, Maheshwari RK. Skin regenerative potentials of curcumin. Biofactors 2013; 39: 141–9. doi: 10.1002/biof.1078 [PubMed] [Cross Ref]60.
Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: consequences and mechanisms. Lancet Oncol 2003; 4: 529–36. [PubMed]61.
Schmidt-Ullrich RK, Dent P, Grant S, Mikkelsen RB, Valerie K. Signal transduction and cellular radiation responses. Radiat Res 2000; 153: 245–57. [PubMed]62.
Schaue D, Kachikwu EL, McBride WH. Cytokines in radiobiological responses: a review. Radiat Res 2012; 178: 505–23. doi: 10.1667/RR3031.1 [PMC free article] [PubMed] [Cross Ref]63.
Siomek A. NF-κB signaling pathway and free radical impact. Acta Biochim Pol 2012; 59: 323–31. [PubMed]64. Chattopadhyay I, Biswas K, Bandyopadhyay U, Banerjee RK. Turmeric and curcumin: biological actions and medicinal applications. Curr Sci 2004; 87: 44–53.
65.
Calabrese V, Bates TE, Mancuso C, Cornelius C, Ventimiglia B, Cambria MT, et al. . Curcumin and the cellular stress response in free radical-related diseases. Mol Nutr Food Res 2008; 52: 1062–73. doi: 10.1002/mnfr.200700316 [PubMed] [Cross Ref]66.
Gupta SC, Patchva S, Aggarwal BB. Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J 2013; 15: 195–218. doi: 10.1208/s12248-012-9432-8 [PMC free article] [PubMed] [Cross Ref]67.
Jelveh S, Kaspler P, Bhogal N, Mahmood J, Lindsay PE, Okunieff P, et al. . Investigations of antioxidant-mediated protection and mitigation of radiation-induced DNA damage and lipid peroxidation in murine skin. Int J Radiat Biol 2013; 89: 618–27. doi: 10.3109/09553002.2013.782450 [PubMed] [Cross Ref]68.
Parshad R, Sanford KK, Price FM, Steele VE, Tarone RE, Kelloff GJ, et al. . Protective action of plant polyphenols on radiation-induced chromatid breaks in cultured human cells. Anticancer Res 1998; 18: 3263–6. [PubMed]69.
Sitton E. Early and late radiation-induced skin alterations. Part I. Mechanism of skin changes. Oncol Nurs Forum 1992; 19: 801–7. [PubMed]70.
Huang MT, Lysz T, Ferraro T, Abidi TF, Laskin JD, Conney AH. Inhibitory effects of curcumin on in vitro lipoxygenase and cyclooxygenase activities in mouse epidermis. Cancer Res 1991; 51: 813–19. [PubMed]71.
Chun KS, Keum YS, Han SS, Song YS, Kim SH, Surh YJ. Curcumin inhibits phorbol ester-induced expression of cyclooxygenase-2 in mouse skin through suppression of extracellular signal-regulated kinase activity and NF-kappaB activation. Carcinogenesis 2003; 24: 1515–24. [PubMed]72.
Okunieff P, Xu J, Hu D, Liu W, Zhang L, Morrow G, et al. . Curcumin protects against radiation-induced acute and chronic cutaneous toxicity in mice and decreases mRNA expression of inflammatory and fibrogenic cytokines. Int J Radiat Oncol Biol Phys 2006; 65: 890–8. [PubMed]73.
Cho JW, Lee KS, Kim CW. Curcumin attenuates the expression of IL-1beta, IL-6, and TNF-alpha as well as cyclin E in TNF-alpha-treated HaCaT cells; NF-kappaB and MAPKs as potential upstream targets. Int J Mol Med 2007; 19: 469–74. [PubMed]74.
Jagetia GC, Rajanikant GK. Effect of curcumin on radiation-impaired healing of excisional wounds in mice. J Wound Care 2004; 13: 107–9. [PubMed]75.
Jagetia GC, Rajanikant GK. Role of curcumin, a naturally occurring phenolic compound of turmeric in accelerating the repair of excision wound, in mice whole-body exposed to various doses of gamma-radiation. J Surg Res 2004; 120: 127–38. doi: 10.1016/j.jss.2003.12.003 [PubMed] [Cross Ref]76.
Jagetia GC, Rajanikant GK. Curcumin treatment enhances the repair and regeneration of wounds in mice exposed to hemibody gamma-irradiation. Plast Reconstr Surg 2005; 115: 515–28. [PubMed]77.
Jagetia GC, Rajanikant GK. Acceleration of wound repair by curcumin in the excision wound of mice exposed to different doses of fractionated γ radiation. Int Wound J 2012; 9: 76–92. [PubMed]
tumeric, curcuma, zalf met sandelhoutolie en curcuma, hoofd- halstumoren, bestraling, dermatitis, huidschade door bestraling
Gerelateerde artikelen




 2
2
Plaats een reactie ...
Reageer op "Zalf met tumeric - curcuma en sandelhoutolie voorkomt veel beter - 75 procent minder - dermatitis - huidschade door bestraling bij patienten met hoofd- halstumoren in vergelijking met babyolie. copy 1"