Uit nieuw onderzoek van het Integraal Kankercentrum Nederland (IKNL) blijkt dat jonge mensen van jonger dan 50 jaar vaker geconfronteerd worden met darmkanker. De analyse van ruim 20.000 patiënten over de periode 1989-2023 laat zien dat het aantal nieuwe darmkankerpatiënten per jaar onder 15- tot 49-jarigen in Nederland significant is gestegen in de periode 1998-2023. In 1998 werden er 6,3 gevallen per 100.000 personen vastgesteld, terwijl dit aantal in 2023 was toegenomen tot 9,5 per 100.000 personen. Dat betekent dat 654 Nederlanders van 15 t/m 49 jaar de diagnose darmkanker kregen in 2023.
Zie deze grafiek gekopieerd uit studierapport:
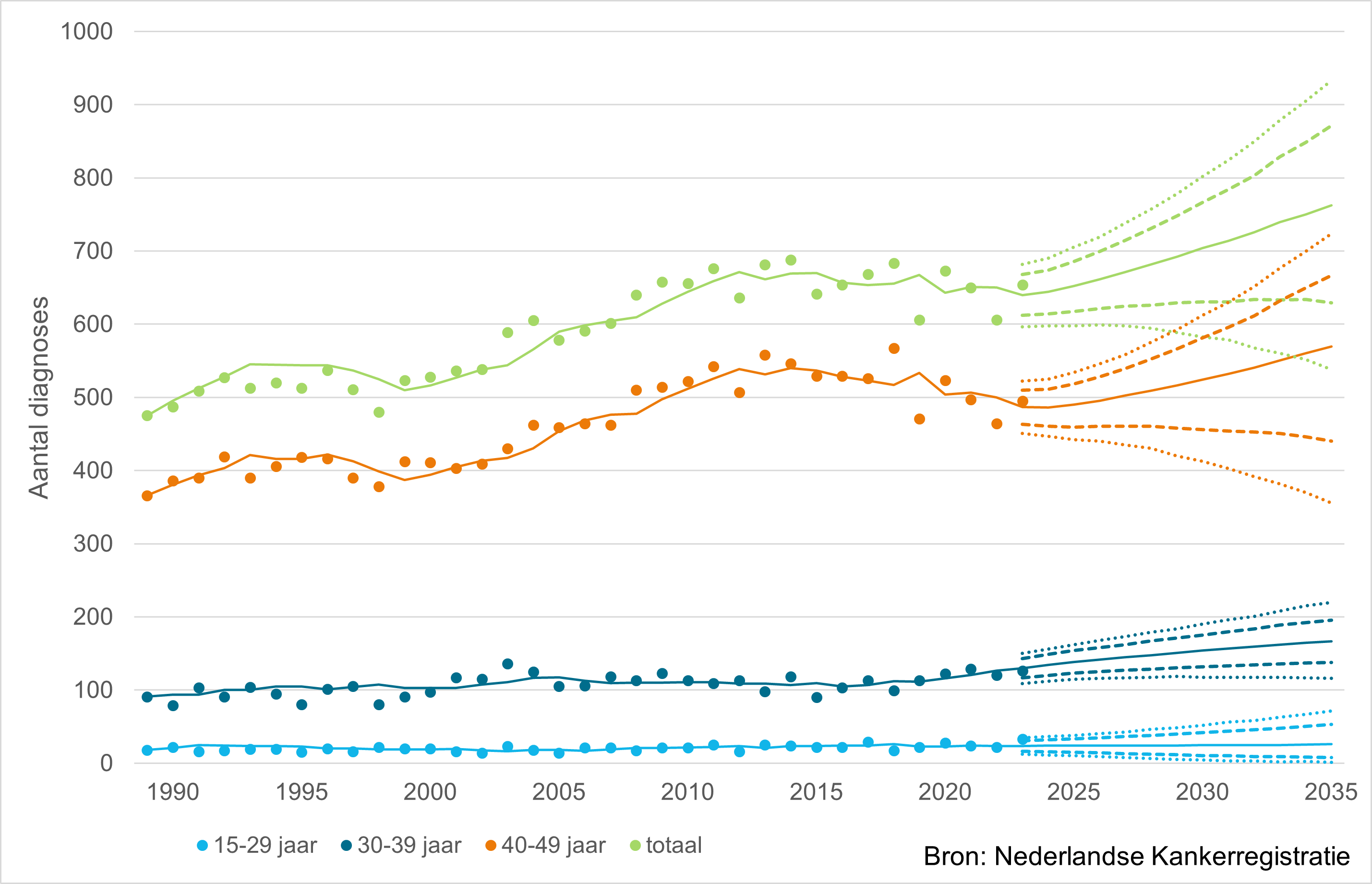
Figuur: Geobserveerde (1989-2023) en verwachte (2024-2035) incidentiecijfers van darmkanker bij mannen en vrouwen jonger dan 50 jaar in de periode 1989-2035 in Nederland, absolute aantallen. De punten zijn de geobserveerde waardes, de lijnen geven de voorspelde waardes (doorgetrokken) en de 80% (gestreept) en 95% (gestippeld) voorspellingsintervallen aan.
Op zich zijn dat in verhouding tot mensen ouder dan 50 jaar die de diagnose darmkanker krijgen geen grote aantallen , maar procentueel: 1,4 procent per jaar afgelopen dertig jaar, is dit behoorlijk veel. Ook wereldwijd is er sprake van een behoorlijke sterke stijging. Zelfs nog meer dan in Nederland. Aldus de onderzoekers van het IKNL onder leiding van Marloes Elferink en collega’s.
De onderzoekers schrijven dat een verandering van leefstijl een grote rol speelt in die stiojging: de afgelopen jaren zijn mensen gemiddeld genomen zwaarder geworden, ze bewegen minder, eten meer bewerkt vlees, drinken meer alcohol en gesuikerde frisdranken. En dat zijn allemaal risicofactoren voor het ontstaan van darmkanker.
Een ander punt van zorg is dat bij klachten van buikpijn en darmklachten bij jongere mensen niet direct gedacht wordt aan darmkanker waardoor wanneer het uiteindelijk toch darmkanker blijkt te zijn dit in een verder gevorderd stadium is dan bij oudere mensen.
Het volledige studieverslag is gepubliceerd in het Nederlands Tijdschrift voor Geneeskunde.
Hier het artikel op de website van het IKNL:
Darmkanker neemt toe bij jonge mensen, maar blijft relatief zeldzaam
Laatst gewijzigd op: 24 april 2025
In Nederland krijgen steeds meer mensen onder de 50 jaar darmkanker. Uit onderzoek van Marloes Elferink van IKNL en collega’s blijkt dat dit aantal de afgelopen decennia is gestegen en naar verwachting verder zal toenemen. Toch blijft darmkanker op jonge leeftijd zeldzaam. De bevindingen, gebaseerd op cijfers uit de Nederlandse Kankerregistratie (NKR), laten zien hoe belangrijk het is dat artsen en patiënten zelf alert zijn en dat er meer onderzoek komt naar oorzaken en manieren om de ziekte te voorkomen.
Het onderzoek, gepubliceerd in het Nederlands Tijdschrift voor Geneeskunde, is uitgevoerd naar aanleiding van internationale rapportages die wijzen op een wereldwijde stijging van darmkanker bij jonge mensen.>>>>>>>lees verder
Ook de Volkskrant heeft er een lezenswaardig artikel aan gewijd:
Darmkanker treft vaker jongeren, stijging baart artsen zorgen: ‘Onze jongste patiënten zijn 18 jaar’
The Lancet publiceerde eerder een studie over dezelfde problematiek. Hier het abstract van deze studie:
Differences in cancer rates among adults born between 1920 and 1990 in the USA: an analysis of population-based cancer registry data
Hyuna Sung, PhDa hyuna.sung@cancer.org ∙ Chenxi Jiang, MPHa ∙ Priti Bandi, PhDa ∙ Adair Minihan, MPHa ∙ Miranda Fidler-Benaoudia, PhDb,c ∙ Farhad Islami, PhDa ∙ et al. Show more
Summary
Background
Trends in cancer incidence in recent birth cohorts largely reflect changes in exposures during early life and foreshadow the future disease burden. Herein, we examined cancer incidence and mortality trends, by birth cohort, for 34 types of cancer in the USA.
Methods
In this analysis, we obtained incidence data for 34 types of cancer and mortality data for 25 types of cancer for individuals aged 25–84 years for the period Jan 1, 2000, to Dec 31, 2019 from the North American Association of Central Cancer Registries and the US National Center for Health Statistics, respectively. We calculated birth cohort-specific incidence rate ratios (IRRs) and mortality rate ratios (MRRs), adjusted for age and period effects, by nominal birth cohort, separated by 5 year intervals, from 1920 to 1990.
Findings
We extracted data for 23 654 000 patients diagnosed with 34 types of cancer and 7 348 137 deaths from 25 cancers for the period Jan 1, 2000, to Dec 31, 2019. We found that IRRs increased with each successive birth cohort born since approximately 1920 for eight of 34 cancers (pcohort<0·050). Notably, the incidence rate was approximately two-to-three times higher in the 1990 birth cohort than in the 1955 birth cohort for small intestine (IRR 3·56 [95% CI 2·96–4·27]), kidney and renal pelvis (2·92 [2·50–3·42]), and pancreatic (2·61 [2·22–3·07]) cancers in both male and female individuals; and for liver and intrahepatic bile duct cancer in female individuals (2·05 [1·23–3·44]). Additionally, the IRRs increased in younger cohorts, after a decline in older birth cohorts, for nine of the remaining cancers (pcohort<0·050): oestrogen-receptor-positive breast cancer, uterine corpus cancer, colorectal cancer, non-cardia gastric cancer, gallbladder and other biliary cancer, ovarian cancer, testicular cancer, anal cancer in male individuals, and Kaposi sarcoma in male individuals. Across cancer types, the incidence rate in the 1990 birth cohort ranged from 12% (IRR1990 vs 1975 1·12 [95% CI 1·03–1·21] for ovarian cancer) to 169% (IRR1990 vs 1930 2·69 [2·34–3·08] for uterine corpus cancer) higher than the rate in the birth cohort with the lowest incidence rate. The MRRs increased in successively younger birth cohorts alongside IRRs for liver and intrahepatic bile duct cancer in female individuals, uterine corpus, gallbladder and other biliary, testicular, and colorectal cancers, while MRRs declined or stabilised in younger birth cohorts for most cancers types.
Interpretation
17 of 34 cancers had an increasing incidence in younger birth cohorts, including nine that previously had declining incidence in older birth cohorts. These findings add to growing evidence of increased cancer risk in younger generations, highlighting the need to identify and tackle underlying risk factors.
Funding
American Cancer Society.
Contributors
HS contributed to study conceptualisation, data curation, investigation, methods, project administration, supervision, validation, and writing of the original manuscript draft and review and editing. CJ contributed to investigation, method, data curation, formal analysis, validation, design of graphs, and reviewing and editing the manuscript. AJ contributed to study conceptualisation, investigation, supervision, and reviewing and editing the manuscript. AM, FI, MF-B, PB and RLS contributed to the investigation and reviewing and editing the manuscript. HS and CJ accessed and verified the underlying data. All authors had full access to all the data in the study, and final responsibility for the decision to submit for publication.
Data sharing
The NAACCR Incidence Data, the SEER Database, and the US Mortality Database (listed in the appendix [p 38]) are non-confidential and publicly accessible data, and can be accessed via a signed Data Use Agreement and distributed through SEER*Stat (version 8.4.2).
Declaration of interests
We declare no competing interests.
Acknowledgments
This study was funded by the Intramural Research Department of the American Cancer Society. We thank all cancer registry staff for their diligence in collecting cancer information, without which this research could not have been conducted. We thank Philip S Rosenberg from National Cancer Institute for the helpful discussion on the statistical methods used in the study.
Supplementary Material (1)
Supplementary appendix
References
Sung, H ∙ Siegel, RL ∙ Rosenberg, PS ∙ et al.
Emerging cancer trends among young adults in the USA: analysis of a population-based cancer registry
Lancet Public Health. 2019; 4:e137-e147Koh, B ∙ Tan, DJH ∙ Ng, CH ∙ et al.
Patterns in cancer incidence among people younger than 50 years in the US, 2010 to 2019
JAMA Netw Open. 2023; 6, e2328171Ugai, T ∙ Sasamoto, N ∙ Lee, HY ∙ et al.
Is early-onset cancer an emerging global epidemic? Current evidence and future implications
Nat Rev Clin Oncol. 2022; 19:656-673di Martino, E ∙ Smith, L ∙ Bradley, SH ∙ et al.
Incidence trends for twelve cancers in younger adults—a rapid review
Br J Cancer. 2022; 126:1374-1386Heer, EV ∙ Harper, AS ∙ Sung, H ∙ et al.
Emerging cancer incidence trends in Canada: the growing burden of young adult cancers
Cancer. 2020; 126:4553-4562Rosenberg, PS ∙ Miranda-Filho, A
Cancer incidence trends in successive social generations in the US
JAMA Netw Open. 2024; 7, e2415731Doll, R
Progress against cancer: an epidemiologic assessment. The 1991 John C. Cassel Memorial Lecture
Am J Epidemiol. 1991; 134:675-688Kreimer, AR ∙ Chaturvedi, AK ∙ Alemany, L ∙ et al.
Summary from an international cancer seminar focused on human papillomavirus (HPV)-positive oropharynx cancer, convened by scientists at IARC and NCI
Oral Oncol. 2020; 108, 104736Tota, JE ∙ Best, AF ∙ Zumsteg, ZS ∙ et al.
Evolution of the oropharynx cancer epidemic in the United States: moderation of increasing incidence in younger individuals and shift in the burden to older individuals
J Clin Oncol. 2019; 37:1538-1546Rosenberg, PS ∙ Check, DP ∙ Anderson, WF
A web tool for age-period-cohort analysis of cancer incidence and mortality rates
Cancer Epidemiol Biomarkers Prev. 2014; 23:2296-2302Lauby-Secretan, B ∙ Scoccianti, C ∙ Loomis, D ∙ et al.
Body fatness and cancer—viewpoint of the IARC Working Group
N Engl J Med. 2016; 375:794-798Fryar, CD ∙ Carroll, MD ∙ Afful, J
Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats
https://www.cdc.gov/nchs/data/hestat/obesity-child-17-18/obesity-child.htm
Date: 2020
Date accessed: May 24, 2024
Reither, EN ∙ Hauser, RM ∙ Yang, Y
Do birth cohorts matter? Age-period-cohort analyses of the obesity epidemic in the United States
Soc Sci Med. 2009; 69:1439-1448Robinson, WR ∙ Keyes, KM ∙ Utz, RL ∙ et al.
Birth cohort effects among US-born adults born in the 1980s: foreshadowing future trends in US obesity prevalence
Int J Obes (Lond). 2013; 37:448-454Fishman, EI ∙ Stokes, A ∙ Preston, SH
The dynamics of diabetes among birth cohorts in the U.S
Diabetes Care. 2014; 37:1052-1059Zheng, H ∙ Echave, P
Are recent cohorts getting worse? Trends in US adult physiological status, mental health, and health behaviors across a century of birth cohorts
Am J Epidemiol. 2021; 190:2242-2255Shah, NS ∙ Lloyd-Jones, DM ∙ Kandula, NR ∙ et al.
Adverse trends in premature cardiometabolic mortality in the United States, 1999 to 2018
J Am Heart Assoc. 2020; 9, e018213Olshansky, SJ ∙ Passaro, DJ ∙ Hershow, RC ∙ et al.
A potential decline in life expectancy in the United States in the 21st century
N Engl J Med. 2005; 352:1138-1145Recalde, M ∙ Pistillo, A ∙ Davila-Batista, V ∙ et al.
Longitudinal body mass index and cancer risk: a cohort study of 2.6 million Catalan adults
Nat Commun. 2023; 14, 3816Murphy, CC ∙ Zaki, TA
Changing epidemiology of colorectal cancer—birth cohort effects and emerging risk factors
Nat Rev Gastroenterol Hepatol. 2024; 21:25-34Browne, AJ ∙ Chipeta, MG ∙ Haines-Woodhouse, G ∙ et al.
Global antibiotic consumption and usage in humans, 2000–18: a spatial modelling study
Lancet Planet Health. 2021; 5:e893-e904Whelan, K ∙ Bancil, AS ∙ Lindsay, JO ∙ et al.
Ultra-processed foods and food additives in gut health and disease
Nat Rev Gastroenterol Hepatol. 2024; 21:406-427Zepeda-Rivera, M ∙ Minot, SS ∙ Bouzek, H ∙ et al.
A distinct Fusobacterium nucleatum clade dominates the colorectal cancer niche
Nature. 2024; 628:424-432Nguyen, LH ∙ Cao, Y ∙ Hur, J ∙ et al.
The sulfur microbial diet is associated with increased risk of early-onset colorectal cancer precursors
Gastroenterology. 2021; 161:1423-1432 e4Mima, K ∙ Kosumi, K ∙ Baba, Y ∙ et al.
The microbiome, genetics, and gastrointestinal neoplasms: the evolving field of molecular pathological epidemiology to analyze the tumor-immune-microbiome interaction
Hum Genet. 2021; 140:725-746Webb, PM ∙ Green, AC ∙ Jordan, SJ
Trends in hormone use and ovarian cancer incidence in US White and Australian women: implications for the future
Cancer Causes Control. 2017; 28:365-370Keyes, KM ∙ Jager, J ∙ Mal-Sarkar, T ∙ et al.
Is there a recent epidemic of women's drinking? A critical review of national studies
Alcohol Clin Exp Res. 2019; 43:1344-1359Ryerson, AB ∙ Schillie, S ∙ Barker, LK ∙ et al.
Vital signs: newly reported acute and chronic hepatitis C cases - United States, 2009–2018
MMWR Morb Mortal Wkly Rep. 2020; 69:399-404Zhang, ER ∙ Pfeiffer, RM ∙ Austin, A ∙ et al.
Impact of HIV on anal squamous cell carcinoma rates in the United States, 2001–2015
J Natl Cancer Inst. 2022; 114:1246-1252Centers for Disease Control and Prevention (CDC)
HIV and AIDS—United States, 1981-2000
MMWR Morb Mortal Wkly Rep. 2001; 50:430-434National Institute of Allergy and Infectious Diseases
Antiretroviral drug discovery and development
US Centers for Disease Control and prevention
HIV surveillance report. HIV diagnoses; 2008–2023; 25–34; all races/ethnicities; both sexes; all transmission categories; United States
https://gis.cdc.gov/grasp/nchhstpatlas/charts.html
Date accessed: May 24, 2024
Haas, CB ∙ Engels, EA ∙ Palefsky, JM ∙ et al.
Severe anal intraepithelial neoplasia trends and subsequent invasive anal cancer in the United States
J Natl Cancer Inst. 2024; 116:97-104Markowitz, LE ∙ Dunne, EF ∙ Saraiya, M ∙ et al.
Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP)
MMWR Recomm Rep. 2007; 56:1-24SEER*Explorer: An interactive website for SEER cancer statistics
Surveillance, Epidemiology, and End Results Program, National Cancer Institute
Rittmeyer, A ∙ Barlesi, F ∙ Waterkamp, D ∙ et al.
Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial
Lancet. 2017; 389:255-265Howlader, N ∙ Forjaz, G ∙ Mooradian, MJ ∙ et al.
The effect of advances in lung-cancer treatment on population mortality
N Engl J Med. 2020; 383:640-649Wagner, C ∙ Carmeli, C ∙ Jackisch, J ∙ et al.
Life course epidemiology and public health
Lancet Public Health. 2024; 9:e261-e269Holford, TR
Understanding the effects of age, period, and cohort on incidence and mortality rates
Annu Rev Public Health. 1991; 12:425-457German, RR ∙ Fink, AK ∙ Heron, M ∙ et al.
The accuracy of cancer mortality statistics based on death certificates in the United States
Cancer Epidemiol. 2011; 35:126-131Gerelateerde artikelen
- Darmkanker komt steeds vaker voor bij ook jonge mensen jonger dan 50 jaar blijkt uit rapport van het IKNL
- Coloscopie lijkt minder effectief in voorkomen en overlijden aan darmkanker dan verwacht volgens internationale gerandomiseerde studie. Echter wie wel een coloscopie had gehad reduceerde de kans op overlijden met 30 tot 50 procent.
- Moleculaire veranderingen plus PD-L1 waarden geven een voorspelling voor de effectiviteit van behandelingen met immunotherapie bij patiënten met gastro-oesofageale adenocarcinoom
- E-nose techniek ruikt verschil tussen darmkanker en darmpoliepen en zou darmkanker vroegtijdig op kunnen sporen, aldus studie uit het VUmc
- Bloedtest kan vroeg darmkanker en voorstadia van darmkanker = kwaadaardige darmpoliepen zichtbaar maken met een betrouwbaarheid van 100 procent voor darmtumoren en 75 procent voor kwaadaardige poliepen van >1 cm.
- In bloed circulerend DNA na chemotherapie of operatie van darmkanker stadium III geeft beduidend slechtere 3-jaars ziektevrije overleving (30 vs 70 procent) en zou als prognosefactor kunnen worden gebruikt voor verdere individuele behandeling
- Analyse van gegevens van in bloed circulerend tumor-DNA bij start en tijdens behandeling blijkt van toegevoegde waarde voor behandelingsopties bij darmkanker na operatie
- Total body MRI gevolgd door verdere specifieke diagnose van uitgezaaide darmkanker is beter en leidt sneller tot nauwkeuriger behandelplan dan standaard diagnose.
- Diagnose: IOBT - FOB test - immunochromatographic fecal occult blood test - ontlastingstest goedkoper en minder belastend voor de patiënt in het opsporen en vaststellen van darmkanker
- Histologische subtype - karakter - van darmkanker en rectumkanker heeft een grote invloed op patroon van hoe en waar uitzaaiingen ontstaan en is van cruciaal belang voor post-operatieve behandelingen en follow-up
- Lynchsyndroom, genafwijking die erfelijke vorm van darmkanker aantoont, zou altijd getest moeten worden bij alle darmkankerpatienten, eierstokkanker, en baarmoederhalskanker en baarmoederkanker
- Fecale Immunochemische Test - FIT - blijkt 90 procent nauwkeurig in voorspellen van wel of geen darmkanker.
- Diagnose: FIT test - Fecal immunochemical Test is gevoeliger en betrouwbaarder, dan bloedtesten voor vroegtijdig opsporen van darmkanker.
- Diagnose: Dubbele ballon enterologisch onderzoek van dunne darm geeft nieuwe mogelijkheden voor diagnostiek en behandeling van bloedingen en andere afwijkingen zoals beginnende kanker in dunne darm.
- Diagnose: Dubbele ballon enterologisch onderzoek van dunne darm standaard procedure in Nederland waaronder de VU Amsterdam en Erasmus Rotterdam en UMC Utrecht.
- Diagnose: colonscopie mist heel vaak (ca. 42%) kanker van de appendix - blinde darm - en lijkt onbetrouwbaar voor diagnose van darmkanker.
- Diagnose technieken bij darmkanker, een overzicht



Plaats een reactie ...
Reageer op "Darmkanker komt steeds vaker voor bij ook jonge mensen jonger dan 50 jaar blijkt uit rapport van het IKNL"