9 januari 2018: lees ook dit artikel:
9 november 2014: Bron: NEJM - DOI: 10.1056/NEJMoa1403108
FOLFOXIRI + Bevacizumab (Avastin) geeft in vergelijking met FOLFIRI betere resultaten op progressie vrije tijd 2,4 maanden (van 9,7 naar 12,1 maanden) langere progressie vrije tijd als eerste lijns behandeling bij patiënten met inoperabele uitgezaaide darmkanker. De mediane overall overleving ging van 25,8 naar 31,1 maanden, een "winst" dus van 5,2 maanden. Maar als je ziet wat de bijwerkingen zijn kun je je afvragen of je als patiënt hier blij mee moet zijn. De graad 3/4 bijwerkingen stegen aanzienlijk. Zo steeg het aantal gevallen van neutropenie van 20% naar 50%, diarree van 10,6% naar 18,8%, stomatitis van 4,3% naar 8,8% en peripherale neuropathie van 0% naar 5%. En dat voor 2,4 maanden progressievrije tijd en 5 maanden langer leven?
De studie is uitgevoerd in 34 ziekenhuizen in italië onder leiding van Fotios Loupakis, MD, PhD, van Azienda Ospedaliero-Universitaria Pisana en Universita di Pisa en gepubliceerd in NEJM - The New England Journal of Medicine.
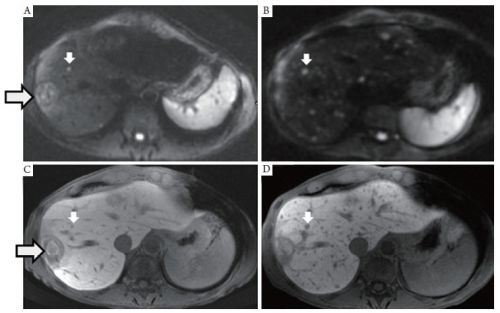
Foto is een beeld van leveruitzaaiingen uit andere studie
Studieresultaten:
A total of 508 patients were randomly assigned to receive either FOLFIRI plus bevacizumab (control group, n = 256) or FOLFOXIRI plus bevacizumab (experimental group, n = 252). Up to 12 cycles of treatment were administered, followed by 5-FU plus bevacizumab until disease progression. Patients had unresectable metastatic colorectal cancer and had not received chemotherapy or biologic therapy for metastatic disease, although 12.6% had received adjuvant chemotherapy earlier in their disease course.
“Demographic and baseline characteristics of the patients were similar in the two groups,” the investigators noted, “but a higher percentage of patients in the experimental group than in the control group had a primary tumor in the right colon (34.9% vs 23.8%, P = .02).” Among all patients, 79.3% had multiple sites of metastases and 20.7% had disease limited to the liver. The median age was 60 in the FOLFIRI group and 60.5 in the FOLFOXIRI group.
Higher Rates of Grade 3/4 Adverse Events
Grade 3/4 neutropenia occurred in 50% of patients receiving FOLFOXIRI vs 20.5% of patients receiving FOLFIRI. Higher rates with FOLFOXIRI vs FOLFIRI also occurred for several other grade 3/4 adverse events, including diarrhea (18.8% vs 10.6 %), febrile neutropenia (8.8% vs 6.3%), stomatitis (8.8% vs 4.3%) and peripheral neuropathy (5.2% vs 0%). The only grade 3/4 adverse event with a higher incidence reported for FOLFIRI was nausea, but the incidences were low and difference slight.
“The incidence of serious adverse events was similar in the two groups (19.7% in the control group and 20.4% in the experimental group, P = .91),” the researchers stated. “A total of 142 (91.6%) of the deaths in the control group and 121 (92.4%) of the deaths in the experimental group were attributed to disease progression. In each group, a similar number of patients died as a result of adverse events (4 [1.6%] in the control group and 6 [2.4%] in the experimental group).”
Het volledige studierapport: Initial Therapy with FOLFOXIRI and Bevacizumab for Metastatic Colorectal Cancer is tegen betaling verkrijgbaar.
Hier het abstract van deze studie:
FOLFOXIRI plus bevacizumab, as compared with FOLFIRI plus bevacizumab, improved the outcome in patients with metastatic colorectal cancer and increased the incidence of some adverse events.
Initial Therapy with FOLFOXIRI and Bevacizumab for Metastatic Colorectal Cancer
N Engl J Med 2014; 371:1609-1618 DOI: 10.1056/NEJMoa1403108
Background
A fluoropyrimidine plus irinotecan or oxaliplatin, combined with bevacizumab (a monoclonal antibody against vascular endothelial growth factor), is standard first-line treatment for metastatic colorectal cancer. Before the introduction of bevacizumab, chemotherapy with fluorouracil, leucovorin, oxaliplatin, and irinotecan (FOLFOXIRI) showed superior efficacy as compared with fluorouracil, leucovorin, and irinotecan (FOLFIRI). In a phase 2 study, FOLFOXIRI plus bevacizumab showed promising activity and an acceptable rate of adverse effects.
Methods
We randomly assigned 508 patients with untreated metastatic colorectal cancer to receive either FOLFIRI plus bevacizumab (control group) or FOLFOXIRI plus bevacizumab (experimental group). Up to 12 cycles of treatment were administered, followed by fluorouracil plus bevacizumab until disease progression. The primary end point was progression-free survival.
Results
The median progression-free survival was 12.1 months in the experimental group, as compared with 9.7 months in the control group (hazard ratio for progression, 0.75; 95% confidence interval , 0.62 to 0.90; P=0.003). The objective response rate was 65% in the experimental group and 53% in the control group (P=0.006). Overall survival was longer, but not significantly so, in the experimental group (31.0 vs. 25.8 months; hazard ratio for death, 0.79; 95% CI, 0.63 to 1.00; P=0.054). The incidences of grade 3 or 4 neurotoxicity, stomatitis, diarrhea, and neutropenia were significantly higher in the experimental group.
Conclusions
FOLFOXIRI plus bevacizumab, as compared with FOLFIRI plus bevacizumab, improved the outcome in patients with metastatic colorectal cancer and increased the incidence of some adverse events. (Funded by the Gruppo Oncologico Nord Ovest and others; ClinicalTrials.gov number, NCT00719797.)
Presented in part at the American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium, San Francisco, January 24–26, 2013, and at the 48th ASCO Annual Meeting, Chicago, May 31–June 4, 2013.
Supported by the Gruppo Oncologico Nord Ovest and the ARCO Foundation. A research grant was provided by F. Hoffmann–La Roche.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank Drs. Manfredi Morvillo and Roberta Savi for administrative support, Drs. Carlotta Antoniotti and Marta Schirripa for clinical support, and the patients and their families.
Source Information
From Azienda Ospedaliero–Universitaria Pisana and Università di Pisa, Pisa (F.L., C. Cremolini, G.M., L.S., A.F.), Istituto Oncologico Veneto, Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS), Padua (S.L., V.Z.), Sapienza Università di Roma (E.C.) and Università Campus Biomedico (G. Tonini), Rome, Azienda Istituti Ospitalieri, Cremona (G. Tomasello), Ospedale San Raffaele, IRCCS, Milan (M.R.), Azienda Ospedaliero–Universitaria Città della Salute e della Scienza, Turin (R.S.), Fondazione Poliambulanza, Brescia (A.Z.), Centro di Riferimento Oncologico, IRCCS, Aviano (A.B.), Ospedale Versilia, Lido di Camaiore (D.A.), Ospedale San Martino, IRCCS, Genoa (S.C.), Azienda Ospedaliera Universitaria Federico II, Naples (C. Carlomagno), Arcispedale Santa Maria Nuova, IRCCS, Reggio Emilia (C.B.), Ospedale Felice Lotti, Pontedera (G.A.), and Azienda Ospedaliero–Universitaria Careggi and Istituto Toscano Tumori, Florence (L.B.) — all in Italy.
Address reprint requests to Dr. Falcone at Azienda Ospedaliero–Universitaria Pisana, Via Roma, 67, 56126 Pisa, Italy, or at alfredo.falcone@med.unipi.it.
Gerelateerde artikelen
- Chemo toedienen in buikholte naast systemische chemo geeft verdubbeling van levensverlenging bij patienten met in buikvlies uitgezaaide darmkanker blijkt uit Nederlandse studie. Vervolgstudie staat open voor nieuwe patienten
- Standaard radiotherapie naast chemo vooraf aan operatie bij rectumkanker geeft zelfde overleving op 5 jaar met meer bijwerkingen in vergelijking met alleen selectieve bestraling als chemo te weinig resultaat geeft copy 1
- Lonsurf (Trifluridine-Tipiracil) plus Bevacizumab (Avastin) geeft betere mediane overall overleving en ziekteprogressievrije tijd dan alleen Trifluridine-Tipiracil bij patienten met recidief van uitgezaaide darmkanker
- Vitamine C hoog gedoseerd naast chemo (FOLFOX +/- bevacizumab) geeft in vergelijking met alleen chemo statistisch significant verschil in mediane overall overleving bij inoperabele onbehandelde uitgezaaide darmkanker met RAS mutatie
- FOLFIRI plus cetuximab geeft betere overall overleving dan Avastin - bevacizumab bij darmkanker KRAS wild type.
- Oxaliplatin plus Xeloda - capecitabine naast bestraling voor operatie van endeldarmkanker geeft alleen maar meer bijwerkingen en geen enkel verschil op ziektevrije tijd en overall overleving en is dus zinloos
- S-1 plus oxaliplatine samen met pembrolizumab geeft hoopvolle resultaten bij patiënten met gevorderde maag / darmkanker met 72 procent objectieve respons copy 1
- mFOLFOX6 - fluorouracil, leucovorin en oxaliplatin (met of zonder radiotherapie) vooraf aan operatie geeft geen betere overall overleving voor gevorderde endeldarmkanker dan alleen fluorouracil (5-FU) plus radiotherapie
- Stoppen met oxaliplatin geeft zelfde resultaten maar minder neuropathie in vergelijking met voortzetting na 6 FOLFOX chemokuren plus panitumumab bij patienten met uitgezaaide gevorderde darmkanker
- CAPOX = Xeloda - capecitabine plus oxaliplatin geeft op 3 jaars meting 10 procent betere ziektevrije tijd (83 vs 73 procent) dan FOLFOX = 5-FU + Leucovarin + oxaliplatin bij darmkanker stadium III
- S-1 plus irinotecan plus bevacizumab versus mFOLFOX6 of CapeOX plus bevacizumab voor uitgezaaide darmkanker geeft betere overall overleving en minder bijwerkingen
- RFA naast systemische chemo geeft betere overall overleving 35.9 procent versus 8.9 procent op 8 jaars meting voor in lever uitgezaaide darmkanker
- Darmkankerpatienten jonger dan 50 jaar krijgen veel te vaak systemische chemo zonder effectiviteit op overleving en ziektevrije tijd in vergelijking met darmkankerpatienten ouder dan 50 jaar.
- FOLFOXIRI + Bevacizumab geeft betere progressievrije tijd (9,7 vs 12,1 maanden) dan FOLFIRI + avastin als eerste lijns behandeling bij inoperabele uitgezaaide darmkanker
- Oxaliplatin voegt niets toe aan effectiviteit bij ouderen met darmkanker en bij darmkanker stadium II
- Chemo bij endeldarmkanker heeft weinig effect op overlevingsduur
- Chemo bij darmkanker: Xeloda - Capecitabine bewezen beter alternatief voor 5-FU bij uitgezaaide darmkanker
- Chemo: Hoe langer gewacht met chemo na operatie van darmkanker tumoren, hoe groter de kans op een recidief, blijkt uit grote meta analyse van 10 gerandomiseerde studies met totaal ruim 15.000 darmkankerpatienten
- Chemo na operatie bij darmkankerpatiënten stadium II lijkt zinloos en levert slechts 5% extra overlevingen.op.
- Historisch overzicht van nut van chemo bij darmkanker na operatie, gebaseerd op een aantal verschillende studies.
- Ibuprofen gaat diarree tegen veroorzaakt door gebruik van Xeloda - Capecitabine volgens ervaringen van kankerpatienten.
- Peritoneal Carcinomatosis - uitzaaiingen in de lymfklieren van de buikholte en op de buikwand vanuit dikke darmkanker geeft slechtere prognose op overleving en ziektevrije tijd dan bij uitzaaiingen in andere organen bij intraveneuze chemo
- Xeloda - Capecitabine is in Europa al jaren toegestaan als eerstelijns behandeling bij postoperatieve behandelingen van al of niet uitgezaaide darmkanker.
- Chemo bij darmkanker: een overzicht van artikelen en belangrijke studies



Plaats een reactie ...
Reageer op "FOLFOXIRI + Bevacizumab geeft betere progressievrije tijd (9,7 vs 12,1 maanden) dan FOLFIRI + avastin als eerste lijns behandeling bij inoperabele uitgezaaide darmkanker"