Aan dit artikel is vele uren gewerkt. Opzoeken, vertalen, op de website plaatsen enz. Als u ons wilt ondersteunen dan kan dat via een al of niet anonieme donatie. Elk bedrag is welkom hoe klein ook. Klik hier als u ons wilt helpen kanker-actueel online te houden. Wij zijn een ANBI organisatie en dus is uw donatie in principe aftrekbaar voor de belasting.
16 april 2015: Nederlandse onderzoekers tonen aan dat uitzaaiingen bij borstkanker vaak te maken heeft met bepaalde tumorafwijkingen. Zo zaaien ER en PR positieve tumoren vaker uit naar de botten en Her2 negatieve tumoren naar andere organen en lymfklieren. Met ook gevolgen voor de prognose op overall overleving.
Maar lees dit verslag maar van hun studie naast het artikel over receptorenexpressie en DNA afwijkingen bij borstkanker daaronder:
17 februari 2015: Bron: Geburtshilfe Frauenheilkd 2015; 75(1): 41-50
DOI: 10.1055/s-0034-1396215
De afgelopen jaren is er bij borstkanker met name veel progressie geboekt in de diagnose en ontdekken van receptorenexpressie en DNA mutaties gerelateerd aan borstkankertumoren. Maar nog te weinig behandelingen worden daar dan ook op afgestemd in de klinische praktijk, aldus vele onderzoekers in binnen- en buitenland. Deels door te weinig bewijs uit goed gekwalificeerde studies, deels door onwetendheid bij de behandelend artsen, vooral in de niet-academische ziekenhuizen, deels ook door te grote ego's van de behandelend artsen, maar vooral door de onderliggende financiële belangen van de farmaceutische bedrijven en ziekenhuizen.
Zie hier een lijst van tot nu toe bekende receptorenafwijkingen en DNA mutaties gerelateerd aan borstkanker:
Table 1 Genes whose mutations could potentially play a role in the pathogenesis or prognosis of breast cancer or affect the therapeutic efficacy of breast cancer treatment [28], [32], [34].
|
AFF2 |
CREBBP |
JAK2 |
NCOR1 |
PTPN22 |
USH2A |
|
AGTR2 |
CSF1R |
KIT |
NCOR2 |
PTPRD |
XBP1 |
|
AKT1 |
CTCF |
KRAS |
NF1 |
RB1 |
|
|
AKT2 |
DCAF4L2 |
LCLAT1 |
NOTCH4 |
RB1CC1 |
|
|
AKT3 |
DDR1 |
LTK |
NRAS |
RELN |
|
|
ARID1A |
EGFR |
LYN |
OR4N4 |
RERG |
|
|
ARID1B |
ERBB2 |
MAGI3 |
OR6A2 |
RPGR |
|
|
ATM |
ERBB3 |
MALAT1 |
PAPSS2 |
RRM2 |
|
|
ATR |
ERBB4 |
MAN2A2 |
PDGFRA |
RUNX1 |
|
|
AURKA |
ESR1 |
MAP2K4 |
PGM2 |
RYR2 |
|
|
BIRC6 |
FBXW7 |
MDM2 |
PIK3CA |
SEPT13 |
|
|
BRAF |
FOXA1 |
MDM4 |
PIK3R1 |
SF3B1 |
|
|
BRCA1 |
FOXC1 |
MED12 |
PIN1 |
SMARCD1 |
|
|
BRCA2 |
FRG1B |
MET |
PLD1 |
SMG1 |
|
|
CASP8 |
FZD7 |
MLL |
POLR1A |
TAB1 |
|
|
CAV1 |
GATA3 |
MLL2 |
PPP2R2A |
TAB2 |
|
|
CBFB |
GPR32 |
MLL3 |
PRKCZ |
TBL1XR1 |
|
|
CCND3 |
HEXA |
MTAP |
PRKDC |
TBX3 |
|
|
CDH1 |
HMGCS2 |
MTPR |
PRKX |
TGFB1 |
|
|
CDKN1B |
IDH3B |
MYBB |
PRLR |
TGFB2 |
|
|
CLCA1 |
INSRR |
MYBL2 |
PRPS2 |
TP53 |
|
|
CLEC19A |
JAK1 |
NCOA3 |
PTEN |
TPH2 |
Meer dan tien jaar na de eerste publicaties van DNA mutaties zijn de analyse methoden zo sterk verbeterd dat op dit moment elke borstkankerpatiënt , zeker met uitgezaaide borstkanker een personalised medicine programma zou kunnen volgen op basis van een goed receptoren- en DNA profiel. Helaas blijft de klinische praktijk ver achter bij wat al bekend is.
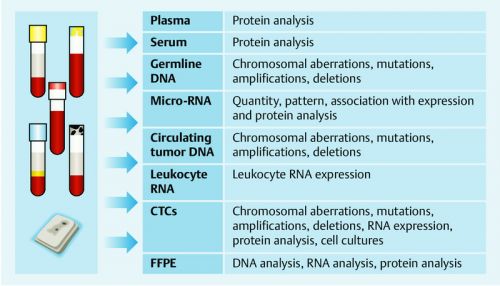
Biomarkers op elk niveau, genetisch, epigenetisch, receptorenexpressie, micro-RNA, proteometics enz. kunnne worden gebruikt voor een gedegen persoonlijke analyse en diagnose. Dit heeft geleid tot veranderingen in de opzet van klinische studies maar te vaak voor te kleine groepen patiënten zodat de resultaten vaak niet worden geaccepteerd voor grotere aantallen patiënten. De screening en registratie van al die afwijkingen in een algemene databank is daarom heel belangrijk om toekomstige klinische studies succesvol en bepalend te laten zijn voor de behandelingen.
De Netwerk groep Preagnant is zo'n groep van ziekenhuizen en onderzoekers die gegevens verzamelen en daaruit weer nieuwe studies ontwerpen en laat zien aan oncologen en behandelaars welke behandelingen en medicijnen verder ontwikkeld zouden moeten worden voor een juiste personalised medicine aanpak.
Dit studierapport: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network vat recente ontwikkelingen samen en beschrijft hoe het Preagnant netwerk een professionele infrastructuur creeërt voor patiënten en professionals, artsen en onderzoekers.
Ik heb maar geen vertaling gemaakt van alles wat in dit studierapport staat beschreven, maar hier het studierapport opgedeeld in enkele belangrijke delen met de referentielijst erbij die correspondeert met de cijfers achter bepaalde citaten.
Prognostic and Predictive Factors in Metastatic Breast Cancer
Source: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
Factors described in some studies as prognostic factors for breast cancer patients with metastatic disease include age, tumor mass, grading, time from primary diagnosis to metastasis, and the site of metastasis [2]. Molecular factors have also been associated with prognosis. Most studies have focused on the prognostic characteristics of the primary tumor and the prognosis for the patient after metastasis. Hormone receptor status, HER2 status and Ki-67 are the most commonly investigated parameters [3]. However, tumor characteristics are known to change during the course of disease [4], [5], [6], [7], [8], [9], [10], [11], and the recommendation to carry out bioptic evaluation of metastases to determine their molecular characteristics has therefore been included in national therapy recommendations [12]. But although obtaining tumor tissue from the breast is relatively uncomplicated, for practical reasons and to avoid complications physicians often object to taking biopsies of metastatic tissue. Etc,: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
- 4 Bogina G, Bortesi L, Marconi M et al. Comparison of hormonal receptor and HER-2 status between breast primary tumours and relapsing tumours: clinical implications of progesterone receptor loss. Virchows Arch 2011; 459: 1-10
- 5 Duchnowska R, Dziadziuszko R, Trojanowski T et al. Conversion of epidermal growth factor receptor 2 and hormone receptor expression in breast cancer metastases to the brain. Breast Cancer Res 2012; 14: R119
- 6 Hoefnagel LD, van de Vijver MJ, van Slooten HJ et al. Receptor conversion in distant breast cancer metastases. Breast Cancer Res 2010; 12: R75
- 7 Hoefnagel LD, Moelans CB, Meijer SL et al. Prognostic value of estrogen receptor α and progesterone receptor conversion in distant breast cancer metastases. Cancer 2012; 118: 4929-4935
- 8 Gong Y, Han EY, Guo M et al. Stability of estrogen receptor status in breast carcinoma: a comparison between primary and metastatic tumors with regard to disease course and intervening systemic therapy. Cancer 2011; 117: 705-713
- 9 Fabi A, Di Benedetto A, Metro G et al. HER2 protein and gene variation between primary and metastatic breast cancer: significance and impact on patient care. Clin Cancer Res 2011; 17: 2055-2064
- 10 Wilking U, Karlsson E, Skoog L et al. HER2 status in a population-derived breast cancer cohort: discordances during tumor progression. Breast Cancer Res Treat 2011; 125: 553-561
- 11 Simon R, Nocito A, Hubscher T et al. Patterns of her-2/neu amplification and overexpression in primary and metastatic breast cancer. J Natl Cancer Inst 2001; 93: 1141-1146
- 12 Kommission Mamma der Arbeitsgemeinschaft für Gynäkologische Onkologie (AGO-Mamma). Diagnosis and treatment of patients with primary and metastatic breast cancer. Online: http://wwwago-onlinede/de/infothek-fuer-aerzte/leitlinienempfehlungen/mamma/maerz-2013/2014 Last update: 28.03.2014; last access: 05.01.2015
Molecular Patterns in Breast Cancer
Source: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
As our knowledge of the human genome increases and the cost of genome-wide analysis decreases, the relationships between genetics, epigenetics, gene expression and protein functions are becoming clearer. The existence of molecular subgroups for breast cancer types and their prognostic relevance based on mRNA measurements were already discussed in the literature more than 10 years ago [13], [14], [15]. One classification differentiates between basal, luminal A, luminal B and HER2-enriched breast cancer subtypes. An attempt was subsequently made to classify these molecular subtypes using known histopathological characteristics [16], [17], [18], [19]. Triple negative tumors (ER negative, PgR negative and HER2 negative) were found to most closely resemble basal tumors. Slow-proliferating (e.g. Ki-67 < 14 %) and hormone receptor-positive tumors generally correspond to luminal A tumors, while hormone receptor-positive tumors with high proliferation rates (e.g. Ki-67 > 14 %) are most closely correlated with luminal B tumors [20], [21], [22]. These cut-offs mirror the biological subtypes. However, other cut-offs (for example 20 %) are also being discussed in clinical practice [23].
Etc.>>>>>>Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
- 13 Perou CM, Sorlie T, Eisen MB et al. Molecular portraits of human breast tumours. Nature 2000; 406: 747-752
- 14 van de Vijver MJ, He YD, vanʼt Veer LJ et al. A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 2002; 347: 1999-2009
- 15 Schmidt M, Fasching PA, Beckmann MW et al. Biomarkers in breast cancer – an update. Geburtsh Frauenheilk 2012; 72: 819-832
- 16 Blows FM, Driver KE, Schmidt MK et al. Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med 2010; 7: e1000279
- 17 Ali AM, Provenzano E, Bartlett JM et al. Prognosis of early breast cancer by immunohistochemistry defined intrinsic sub-types in patients treated with adjuvant chemotherapy in the NEAT/BR9601 trial. Int J Cancer 2013; 133: 1470-1478
- 18 Sotiriou C, Pusztai L. Gene-expression signatures in breast cancer. N Engl J Med 2009; 360: 790-800
- 19 Sotiriou C, Wirapati P, Loi S et al. Gene expression profiling in breast cancer: understanding the molecular basis of histologic grade to improve prognosis. J Natl Cancer Inst 2006; 98: 262-272
- 20 Cheang MC, Chia SK, Voduc D et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 2009; 101: 736-750
- 21 Fasching PA, Heusinger K, Haeberle L et al. Ki67, chemotherapy response, and prognosis in breast cancer patients receiving neoadjuvant treatment. BMC Cancer 2011; 11: 486
- 22 Keam B, Im SA, Lee KH et al. Ki-67 can be used for further classification of triple negative breast cancer into two subtypes with different response and prognosis. Breast Cancer Res 2011; 13: R22
- 23 Yerushalmi R, Woods R, Ravdin PM et al. Ki67 in breast cancer: prognostic and predictive potential. Lancet Oncol 2010; 11: 174-183
- 24 Venter JC, Adams MD, Myers EW et al. The sequence of the human genome. Science 2001; 291: 1304-1351
- 25 Lander ES, Linton LM, Birren B et al. Initial sequencing and analysis of the human genome. Nature 2001; 409: 860-921
- 26 1000 Genomes Project Consortium. Abecasis GR, Auton A et al. An integrated map of genetic variation from 1,092 human genomes. Nature 2012; 491: 56-65
- 27 Fasching PA, Ekici AB, Wachter DL et al. Breast cancer risk – from genetics to molecular understanding of pathogenesis. Geburtsh Frauenheilk 2013; 73: 1228-1235
Genetic variants as prognostic or predictive factors
Source: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
Another genetic tumor change can consist of an increase or decrease in the number of gene copies. In a large investigation carried out as part of the METABRIC study, the number of gene copies and the associated gene expressions were determined for every gene [29]. This allowed positions to be identified in the genome where changes in gene copy numbers and an associated change in gene expression occurred most commonly. Genes in which such changes occurred include ZNF703, PTEN, MYC, CCND1, MDM2, ERBB2, CCNE1, MDM1, MDM4, CDK3, CDK4, CAMK1D, PI4KB and NCOR1 (amplifications) and PPP2R2A, MTAP und MAP2K4 (deletions). The strongest association was found between amplification in the genes HER2 (ERBB2) and cyclin D1 (CCND1). Etc.>>>>>Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
- 28 Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature 2012; 490: 61-70
- 29 Curtis C, Shah SP, Chin SF et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 2012; 486: 346-352
- 30 Loibl S, von Minckwitz G, Schneeweiss A et al. PIK3CA mutations are associated with lower rates of pathologic complete response to anti-human epidermal growth factor receptor 2 (her2) therapy in primary HER2-overexpressing breast cancer. J Clin Oncol 2014; 32: 3212-3220
- 31 Baselga J, Piccart M, Gnant M et al. Minimal molecular alteration in PI3KCA, FGFR1 and CCND1 is associated with increased benefit from everolimus in hormone receptor-positive, HER2-advanced breast cancer: Insights from the BOLERO-2 trial. Eur J Cancer 2013; 49: S404-S405
- 32 Ellis MJ, Ding L, Shen D et al. Whole-genome analysis informs breast cancer response to aromatase inhibition. Nature 2012; 486: 353-360
- 33 Griffith OL, Griffith M, Luo J et al. Prognostic effects of gene mutation in estrogen receptor positive breast cancer. San Antonio Breast Cancer Symposium 2014; Abstract No. S1–02.
- 34 Shah SP, Roth A, Goya R et al. The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature 2012; 486: 395-399
Significance of genetic germline variants
Source: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
A patientʼs genetic heredity can be associated with a specific molecular breast cancer subtype. The most famous examples of this are patients with the BRCA1 mutation. If a patient with the BRCA1 mutation develops breast cancer, the probability that this cancer will be triple negative is more than 50 % [27], [35], [36]. Other low-penetrance genetic variants reported in the literature were also found to be associated with a specific molecular subtype [37], [38], [39], [40], [41], [42], [43], [44], [45]. Some of them are similar to BRCA1 and BRCA2 in that they play important roles in both breast cancer and ovarian cancer [46], [47], [48]. Table 2 Breast cancer studies which have integrated molecular tests in their study design or use them as predictors for the primary study goal (* relevant for therapy or study means that the results of biomarker tests affected the choice of therapy or the study design over and above stratification or subgroup analysis; ** in some of these studies, inoperable locally advanced disease was sufficient for inclusion in the study). Etc.>>>>>> Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
|
Study name |
Test |
Test results relevant for therapy or study* |
Drug |
Therapy setting |
|---|---|---|---|---|
|
BRIGHTNESS (NCT02032277) |
germline DNA testing for BRCA1/2 mutation |
veliparib |
neoadjuvant |
|
|
Olympia (NCT02032823) |
germline DNA testing for BRCA1/2 mutation |
X |
olaparib |
adjuvant/post-neoadjuvant |
|
EMBRACA (NCT01945775) |
germline DNA testing for BRCA1/2 mutation |
X |
talazoparib |
1st–3rd line metastasized** |
|
ABRAZO (NCT02034916) |
germline DNA testing for BRCA1/2 mutation |
X |
talazoparib |
4th+ line metastasized** |
|
Neoadjuvant BYL719 vs. BKM120 Study (NCT01923168) |
tumor PI3K testing |
X |
buparlisib (BKM120)/alpelisib (BYL719) |
neodjuvant |
|
PRESENT (NCT01479244) |
HLA testing/HER2 testing |
X |
nelipepimut-S |
adjuvant |
|
DETECT III/IV (NCT01619111) |
measurement of HER2 and ER expression in CTCs |
X |
lapatinib, everolimus, eribulin |
|
|
FERGI (NCT01437566) |
tumor PI3K testing |
pictilisib |
metastasized** |
|
|
BT062 (EudraCT No. 2013–003 252–20) |
TNBC, CD138 expression |
X |
indatuximab, ravtansine |
metastasized |
|
Belle 2/3/4 (NCT01610284, NCT01633060, NCT01572727) |
tumor PI3K testing |
buparlisib (BKM120) |
metastasized** |
|
|
GLOW (NCT01202591) |
tumor FGFR1 amplification |
X |
AZD4547 |
metastasized** |
|
ADAPT (NCT01817452, NCT01745965) |
21-gene expression testing; serial gene expression testing |
X |
various |
neoadjuvant/adjuvant |
|
PreFace (NCT01908556) |
genome-wide germline genotyping |
letrozole |
adjuvant |
|
|
SUCCESS C (NCT00847444) |
CTC determination |
X |
exemestan/ |
adjuvant |
- 35 Couch FJ, Hart SN, Sharma P et al. Inherited mutations in 17 breast cancer susceptibility genes among a large triple-negative breast cancer cohort unselected for family history of breast cancer. J Clin Oncol 2014; DOI: 10.1200/JCO.2014.57.1414
- 36 Lakhani SR, Reis-Filho JS, Fulford L et al. Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res 2005; 11: 5175-5180
- 37 Fasching PA, Weihbrecht S, Haeberle L et al. HER2 and TOP2A amplification in a hospital-based cohort of breast cancer patients: associations with patient and tumor characteristics. Breast Cancer Res Treat 2014; 145: 193-203
- 38 Broeks A, Schmidt MK, Sherman ME et al. Low penetrance breast cancer susceptibility loci are associated with specific breast tumor subtypes: findings from the Breast Cancer Association Consortium. Hum Mol Genet 2011; 20: 3289-3303
- 39 Purrington KS, Slager S, Eccles D et al. Genome-wide association study identifies 25 known breast cancer susceptibility loci as risk factors for triple negative breast cancer. Carcinogenesis 2014; 35: 1012-1019
- 40 Stevens KN, Fredericksen Z, Vachon CM et al. 19p13.1 is a triple negative-specific breast cancer susceptibility locus. Cancer Res 2012; 72: 1795-1803
- 41 Garcia-Closas M, Couch FJ, Lindstrom S et al. Genome-wide association studies identify four ER negative-specific breast cancer risk loci. Nat Genet 2013; 45: 392-398
- 42 Milne RL, Benitez J, Nevanlinna H et al. Risk of estrogen receptor-positive and -negative breast cancer and single-nucleotide polymorphism 2q35-rs13387042. J Natl Cancer Inst 2009; 101: 1012-1018
- 43 Figueroa JD, Garcia-Closas M, Humphreys M et al. Associations of common variants at 1p11.2 and 14q24.1 (RAD51L1) with breast cancer risk and heterogeneity by tumor subtype: findings from the Breast Cancer Association Consortium. Hum Mol Genet 2011; 20: 4693-4706
- 44 French JD, Ghoussaini M, Edwards SL et al. Functional variants at the 11q13 risk locus for breast cancer regulate cyclin D1 expression through long-range enhancers. Am J Hum Genet 2013; 92: 489-503
- 45 Stevens KN, Vachon CM, Lee AM et al. Common breast cancer susceptibility loci are associated with triple-negative breast cancer. Cancer Res 2011; 71: 6240-6249
- 46 Fasching PA, Gayther S, Pearce L et al. Role of genetic polymorphisms and ovarian cancer susceptibility. Mol Oncol 2009; 3: 171-181
- 47 Bolton KL, Tyrer J, Song H et al. Common variants at 19p13 are associated with susceptibility to ovarian cancer. Nat Genet 2010; 42: 880-884
- 48 Antoniou AC, Wang X, Fredericksen ZS et al. A locus on 19p13 modifies risk of breast cancer in BRCA1 mutation carriers and is associated with hormone receptor-negative breast cancer in the general population. Nat Genet 2010; 42: 885-892
- 49 Fasching PA, Loehberg CR, Strissel PL et al. Single nucleotide polymorphisms of the aromatase gene (CYP19A1), HER2/neu status, and prognosis in breast cancer patients. Breast Cancer Res Treat 2008; 112: 89-98
- 50 Azzato EM, Tyrer J, Fasching PA et al. Association between a germline OCA2 polymorphism at chromosome 15q13.1 and estrogen receptor-negative breast cancer survival. J Natl Cancer Inst 2010; 102: 650-662
- 51 Fasching PA, Pharoah PD, Cox A et al. The role of genetic breast cancer susceptibility variants as prognostic factors. Hum Mol Genet 2012; 21: 3926-3939
- 52 Weischer M, Nordestgaard BG, Pharoah P et al. CHEK2*1100delC heterozygosity in women with breast cancer associated with early death, breast cancer-specific death, and increased risk of a second breast cancer. J Clin Oncol 2012; 30: 4308-4316
- 53 Vachon CM, Scott CG, Fasching PA et al. Common breast cancer susceptibility variants in LSP1 and RAD51L1 are associated with mammographic density measures that predict breast cancer risk. Cancer Epidemiol Biomarkers Prev 2012; 21: 1156-1166
- 54 Lindstrom S, Thompson DJ, Paterson AD et al. Genome-wide association study identifies multiple loci associated with both mammographic density and breast cancer risk. Nat Commun 2014; 5: 5303
- 55 Fasching PA, Heusinger K, Loehberg CR et al. Influence of mammographic density on the diagnostic accuracy of tumor size assessment and association with breast cancer tumor characteristics. Eur J Radiol 2006; 60: 398-404
- 56 Heusinger K, Jud SM, Haberle L et al. Association of mammographic density with hormone receptors in invasive breast cancers: results from a case-only study. Int J Cancer 2012; 131: 2643-2649
- 57 Heusinger K, Jud SM, Haberle L et al. Association of mammographic density with the proliferation marker Ki-67 in a cohort of patients with invasive breast cancer. Breast Cancer Res Treat 2012; 135: 885-892
- 58 Hack CC, Haberle L, Geisler K et al. Mammographic density and prediction of nodal status in breast cancer patients. Geburtsh Frauenheilk 2013; 73: 136-141
- 59 Murdter TE, Schroth W, Bacchus-Gerybadze L et al. Activity levels of tamoxifen metabolites at the estrogen receptor and the impact of genetic polymorphisms of phase I and II enzymes on their concentration levels in plasma. Clin Pharmacol Ther 2011; 89: 708-717
- 60 Schroth W, Hamann U, Fasching PA et al. CYP2D6 polymorphisms as predictors of outcome in breast cancer patients treated with tamoxifen: expanded polymorphism coverage improves risk stratification. Clin Cancer Res 2010; 16: 4468-4477
- 61 Schroth W, Goetz MP, Hamann U et al. Association between CYP2D6 polymorphisms and outcomes among women with early stage breast cancer treated with tamoxifen. JAMA 2009; 302: 1429-1436
- 62 Province MA, Goetz MP, Brauch H et al. CYP2D6 genotype and adjuvant tamoxifen: meta-analysis of heterogeneous study populations. Clin Pharmacol Ther 2014; 95: 216-227
- 63 Robson ME, Tutt A, Balmaña J et al. OlympiA, Neo-Olympia and OlympiAD: randomized phase III trials of olaparib in patients (pts) with breast cancer (BC) and a germline BRCA1/2 mutation (gBRCAm). San Antonio Breast Cancer Symposium 2014; Abstract No. OT1-1 – 04.
- 64 Turner NC, Balmana J, Domchek SM et al. A phase 2, 2-stage, 2-cohort study of the oral PARP inhibitor BMN 673 in patients with germline BRCA mutation and locally advanced and/or metastatic breast cancer (ABRAZO study). San Antonio Breast Cancer Symposium 2014; Abstract No. OT1-1 – 14.
- 65 Litton JK, Blum JL, Eiermann W et al. A phase 3, open-label, randomized, parallel, 2-arm multi-center study of the oral PARP inhibitor BMN 673 versus physicianʼs choice in germline BRCA mutation subjects with locally advanced and/or metastatic breast cancer (EMBRACA study). San Antonio Breast Cancer Symposium 2014; Abstract No. OT1-1 – 12.
Circulating Tumor Cells and Circulating Tumor Nucleic Acids
Source: Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
The presence of circulating tumor cells (CTC) in plasma has been consistently associated with prognosis in patients with metastasized breast cancer [66], [67], [68], [69]. The presence of CTCs was found to be an independent prognostic factor even in the non-metastatic setting [70]. The next logical step was to determine the molecular properties of circulating tumor cells [71], [72]. Several clinical studies are currently looking at whether this could help with treatment planning and offer useful information for prognosis [73], [74], [75], [76]. However, isolating the CTCs is still relatively expensive and time-consuming and requires large, cost-intensive equipment which is expensive to run.
A less expensive approach could be to analyze circulating nucleic acids. Tumor cells in the body release small amounts of DNA into the bloodstream, known as circulating DNA (ctDNA). This process was first described in 1948 [77], [78]. Etc.>>>>>>>>>Biomarkers in Patients with Metastatic Breast Cancer and the PRAEGNANT Study Network
- 66 Muller V, Riethdorf S, Rack B et al. Prognostic impact of circulating tumor cells assessed with the CellSearch System and AdnaTest Breast in metastatic breast cancer patients: the DETECT study. Breast Cancer Res 2012; 14: R118
- 67 Wallwiener M, Hartkopf AD, Baccelli I et al. The prognostic impact of circulating tumor cells in subtypes of metastatic breast cancer. Breast Cancer Res Treat 2013; 137: 503-510
- 68 Bidard FC, Peeters DJ, Fehm T et al. Clinical validity of circulating tumour cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol 2014; 15: 406-414
- 69 Cristofanilli M, Budd GT, Ellis MJ et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 2004; 351: 781-791
- 70 Rack B, Schindlbeck C, Juckstock J et al. Circulating tumor cells predict survival in early average-to-high risk breast cancer patients. J Natl Cancer Inst 2014;
- 71 Fehm T, Becker S, Duerr-Stoerzer S et al. Determination of HER2 status using both serum HER2 levels and circulating tumor cells in patients with recurrent breast cancer whose primary tumor was HER2 negative or of unknown HER2 status. Breast Cancer Res 2007; 9: R74
- 72 Fehm T, Muller V, Aktas B et al. HER2 status of circulating tumor cells in patients with metastatic breast cancer: a prospective, multicenter trial. Breast Cancer Res Treat 2010; 124: 403-412
- 73 Melcher CA, Janni W, Rack B et al. DETECT III – a multicenter, randomized, phase III study to compare standard therapy alone versus standard therapy plus lapatinib in patients with initially HER2-negative metastatic breast cancer and HER2-positive circulating tumor cells. Eur J Cancer 2012; 48: S95-S96
- 74 Hagenbeck C, Melcher CA, Janni JW et al. DETECT III: a multicenter, randomized, phase III study to compare standard therapy alone versus standard therapy plus lapatinib in patients (pts) with initially HER2-negative metastatic breast cancer but with HER2-positive circulating tumor cells (CTC). J Clin Oncol 2012; 30 (Suppl.) Abstr. TPS1146
- 75 Melcher C, Schochter F, Albrecht S et al. DETECT IV – a multicenter, single arm, phase II study evaluating the efficacy of Everolimus in combination with endocrine therapy in patients with HER2-negative, hormone-receptor positive metastatic breast cancer and exclusively HER2-negative circulating tumor cells (CTCs). Oncol Res Treat 2014; 37: 29-29
- 76 Albrecht S, Schochter F, Melcher C et al. DETECT III – a multicenter, randomized, phase III trial to assess efficacy of lapatinib in patients with HER2-negative metastatic breast cancer and HER2-positive circulating tumor cells (CTCs). Oncol Res Treat 2014; 37: 29-29
- 77 Mandel P, Metais P. Les acides nucleiques du plasma sanguin chez lʼhomme. C R Seances Soc Biol Fil 1948; 142: 241-243
- 78 Haber DA, Velculescu VE. Blood-based analyses of cancer: circulating tumor cells and circulating tumor DNA. Cancer Discov 2014; 4: 650-661
- 79 Dixon JM, Turnbull AK, Fan C et al. In-depth genomic analysis of ER+ breast cancers during development of endocrine resistance. San Antonio Breast Cancer Symposium 2014; Abstract No. S1-05.
- 80 Rothe F, Laes JF, Lambrechts D et al. Plasma circulating tumor DNA as an alternative to metastatic biopsies for mutational analysis in breast cancer. Ann Oncol 2014; 25: 1959-1965
- 81 Krop I, Johnston S, Mayer IA et al. The FERGI phase II study of the PI3 K inhibitor pictilisib (GDC-0941) plus fulvestrant vs. fulvestrant plus placebo in patients with ER+, aromatase inhibitor (AI)- resistant advanced or metastatic breast cancer. San Antonio Breast Cancer Symposium 2014; Abstract No. S2–02.
- 82 Fasching PA, Decker T, Schneeweiss A et al. Breast cancer treatment with everolimus and exemestane for ER+ women – Results of the 2nd interim analysis of the non-interventional trial BRAWO. European Society of Medical Oncology Meeting (ESMO). 2014; Abstract No. LBA9.
Gerelateerde artikelen
- Elacestrant geeft betere ziekteprogressievrije tijd bij uitgezaaide borstkanker (type ER plus / HER2 negatief en met ESR1 mutatie) na falen van CDK4/6 remmer plus hormoontherapie
- ctDNA, een bloedtest op circulerend DNA geeft 98 procent betrouwbaarheid bij borstkankerpatienten en bewijst effectiviteit van gebruik in de klinische praktijk bij studie met 350 patienten
- Sacituzumab govitecan (Trodelvy) een anti-lichaam medicijn geeft zeer goede resultaten bij borstkankerpatiënten met voorbehandelde uitgezaaide triple-negatieve borstkanker met TROP-2 mutatie in vergelijking met chemotherapie copy 1
- Borstkanker: BRIP1 mutatie geeft uitstekende respons op olaparib bij uitgezaaide HR-positieve, HER2-negatieve borstkanker blijkt uit casestudie copy 1
- CDK4 en 6-remmers - palbociclib, ribociclib en abemaciclib - zijn mogelijk minder effectief bij patiënten met mutaties in deze genen BRCA1/2-ATM-CHEK2 in vergelijking met wild types van genoemde genen
- Borstkanker: Receptorstatus van primaire tumor bij vrouwen met uitgezaaide borstkanker verschilt gemiddeld 31 procent (range 20 tot 65 procent bij HER2+ subtype) met die van de receptorstatus van de uitzaaiingstumor
- Durvalumab met Olaparib en Paclitaxel geeft 17 procent betere complete remissies in vergelijking met alleen chemo bij vrouwen met borstkanker stadium II / III hoog risico, maar ook bij HER2 positief en triple negatief
- Genetische testen uitvoeren bij alle vrouwen met borstkanker kan jaarlijks veel doden aan eierstokkanker en borstkanker voorkomen en is veel kosten effectiever vergeleken met genetisch testen op basis van klinische criteria of familiegeschiedenis
- Borstkanker: Vrouwen met hormoongevoelige borstkanker in leeftijd van de overgang - 45 tot 50 jaar - zijn meer gebaat bij eerst aromastase remmers ipv tamoxifen als de eierstokken nog aanwezig zijn
- HRDetect voorspelt voor 98 procent of BRCA mutaties oorzaak zijn van borstkanker en 20 procent zou daarmee gevoelig zijn voor antineoplaston medicijnen zoals olaparib
- Genezend medicijn - Parpremmer voor vormen van kanker met verstoorde BRCA - PD-functie ligt al jaren op de plank maar mag niet aan patienten worden gegeven
- Immuuntherapie met combinatiebehandeling van nivolumab en ipilimumab zou voor patienten met zogeheten metaplastische borstkanker een behandelingsoptie kunnen zijn blijkt uit kleinschalige studie copy 1
- Linda, diagnose borstkanker, ervaart dat ook haar kanker uniek is en zoekt samen met oncologe beste behandelingen via o.a. biomoleculair profile onderzoek bij Caris.
- Borstkanker wordt vaak overbehandeld. Erasmus MC doet daar wat aan via de Sonia studie.
- Borstkanker: bloedtest na behandeling van borstkanker waarbij resistentie optreedt traceert HER2 mutaties die soms ontstaan tijdens de behandeling met Kinaseremmers en hormoontherapie
- Borstkanker: Richtlijnen voor aanvullende behandelingen bij borstkanker, maar geldt ook voor andere vormen van kanker, officieel gepubliceerd in Amerika op basis van studiebewijs copy 2
- Borstkanker: Snel de beste medicijnen bij alle patiënten. Te beginnen met Olaparib.
- Borstkanker: PI3K remmer buparlisib naast fulvestrant geeft 30 tot 50 procent langere ziekteprogressievrije tijd maar wel meer bijwerkingen bij gevorderde borstkanker
- Borstkanker: Palpociclib plus fulvestrand geeft langere overall overleving en progressievrije ziekte dan alleen fulvesrtrand bij hormoonresistente borstkanker
- Borstkanker: DNA mutaties die een rol spelen bij ontstaan van borstkanker zijn verschillend bij Afrikaanse vrouwen dan bij Europees/Amerikaanse vrouwen blijkt uit grote case studie
- Borstkanker: Immuuntherapie in fase II studie voor patienten met triple negatieve borstkanker met nivolumab gestart in Anthonie van Leeuwenhoek ziekenhuis per 3 september 2015.
- Borstkanker: Voorspellende biomoleculaire markers en DNA mutaties bij borstkanker en uitgezaaide borstkanker: een overzichtstudie vanuit het Preagnant netwerk
- Borstkanker: 4-genentest voorspelt binnen 14 dagen wel of niet aanslaan van hormoonbehandeling met letrozole - femara
- Borstkanker: Enzalutamide - Xtandi geeft spectaculaire resultaten bij gevorderde triple negatieve borstkanker (stadium 4) met ook een positieve expressie van de hormoonreceptor.
- Borstkanker: CD8 positieve expressie plus T-cel infiltratie in tumor en beenmerg voorspellen als markers een significant verlaagd risico - 21 tot 57 procent - op overlijden aan borstkanker, zowel bij ER-HER2 pos als ER neg. vormen van borstkanker
- Borstkanker: PKI3CA enzym expressie bepalend voor verwacht resultaat van chemo behandeling bij borstkanker en is gerelateerd aan HER2 status en hormoonstatus copy 1
- Borstkanker: Pertuzumab - Perjeta door FDA goedgekeurd als eerstelijns behandeling immuuntherapie bij operabele borstkanker HER-2 positief na uitstekende resultaten uit fase 3 APHINITY studie copy 1



Plaats een reactie ...
Reageer op "Borstkanker: Voorspellende biomoleculaire markers en DNA mutaties bij borstkanker en uitgezaaide borstkanker: een overzichtstudie vanuit het Preagnant netwerk"