5 oktober 2017: Bron:
T1 of T2)
Na een mediane follow-up van 9.3 jaar, was de 10-jaars overall overleving 86.3% in de SLND-alleen groep (alleen schildwachtklier is weggehaald) versus 83.6% in de ALND group (alle lymfklieren in de oksel wroden weggehaald) (HR = 0.85, 1-sided 95% confidence interval = 0–1.16; noninferiority P = .02). Tien jaars ziektevrije tijd was 80.2% (SLND) versus 78.2% (ALND) (HR = 0.85, 95% CI = 0.62–1.17, P = .32).
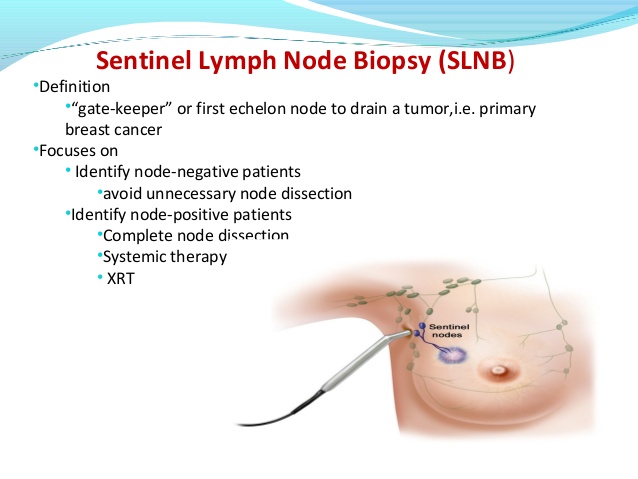
In deze studie werden 891 vrouwen tussen mei 1999 en december 2004 gerandomiseerd ingedeeld om of alleen SLND (n = 446) of ALND (n = 445) te ondergaan. Alle patiënten hadden een borstbesparende operatie gepland, een geplande hele borstbestraling en aanvullende systemische therapie; "Third-field" bestraling was verboden. Het primaire doel was de algehele overleving te meten met een niet-inferioriteitsgevaarverhouding (HR) in een marge van 1,3. Zie studieprotocol: NCT00003855
Het volledige studierapport, gepubliceerd in JAMA: Effect of Axillary Dissection vs No Axillary Dissection on 10-Year Overall Survival Among Women With Invasive Breast Cancer and Sentinel Node Metastasis is tegen betaling in te zien.
Hier het abstract van de studie:
Among women with T1 or T2 invasive primary breast cancer, no palpable axillary adenopathy, and 1 or 2 sentinel lymph nodes containing metastases, 10-year overall survival for patients treated with sentinel lymph node dissection alone was noninferior to overall survival for those treated with axillary lymph node dissection. Based on 10 years outcome
Gerelateerde artikelen
- Borstreconstructie mag voortaan door plastische chirurgen worden bepaald of het nodig is of niet. Ziektekostenverzekeraars veranderen machtiging tot borstreconstructie.
- SIRA, een RFA elektrochirurgisch apparaat dat intraoperatief RFA geeft bij borstbesparende operatie is door FDA goedgekeurd en eerste borstkankerpatient is er succesvol mee behandeld
- Radio Frequency Ablation (RFA) en Cryosurgery (bevriezingstechniek) blijken ook bij operabele niet uitgezaaide borstkanker uitstekende operatietechnieken
- Borstsparende operatie van mucineuze borstkanker geeft een lager risico op overlijden door welke oorzaak dan ook in vergelijking met volledige borstverwijdering (mastectomy
- Cryosurgery plus 1x ipilimumab vooraf aan operatie van operabele borstkanker stimuleert immuunreactie en geeft betere therapeutische resultaten copy 1
- Eerst operatie van borst voor HER2 positieve borstkanker stadium IV gevolgd door systemische behandelingen geeft 44 procent meer overall overlevingen dan systemische behandelingen zonder operatie
- Weghalen van levertumoren bij geselecteerde groep patienten met uitgezaaide borstkanker geeft langere ziektevrije tijd en betere overall overleving op 5 jaar
- Alleen schildwachtklier verwijderen bij borstkanker geeft na 10 jaar zelfde resultaten op overall overleving en kans op recidief dan volledige okselklierdissectie
- Beste borstkankeroperatie techniek - echogeleide operatie - wordt nog te weinig ingezet in Nederland. 17 procent loopt onnodig risico op recidief of hersteloperatie copy 1
- Borstsparende operatie plus bestraling geeft 20 procent betere 10-jaars ziektevrije overleving dan volledige borstamputatie zonder bestraling voor borstkanker
- CPM - contralaterale profylactische mastectomie - verwijdering van gezonde borst naast operatieve verwijdering van borst met kanker geeft nauwelijks verschil in overlevingskansen
- MarginProbe bewijst grote waarde voor patiënten met operabele borstkanker. Noodzaak van hersteloperatie verminderde door MarginProbe met 50 procent
- Operatie: Een ultra sound - echografisch - geleide operatie lijkt beter in staat om volledig borstkanker tumoren te verwijderen en spaart meer gezond weefsel dan een standaard operatie geleid door palpatie (op gevoel van de chirurg).
- Operatie: Harvard professoren hadden al in 2003 grote twijfels bij bioptie en operatie van borstkanker.
- Cryosurgery - bevriezingstechniek - wordt soms wel toegepast bij borstkanker om een recidief te voorkomen
- Operatie: De kans op een recidief van borstkanker na operatie en schone schildwachtklieren is veel groter dan verwacht blijkt uit grote Zweedse studie.
- Operatie: Een operatieve verwijdering van de primaire tumor bij reeds uitgezaaide borstkanker geeft toch significant betere overlevingskansen, vooral bij vrouwen met alleen uitzaaiingen in de botten.
- Operatie: Routinematige operatie van de okselklieren bij beginnende borstkanker is onnodig en beinvloed kwaliteit van leven onnodig als er verder geen aantoonbare uitzaaiingen zijn en schildwachtklier schoon is. Artikel geplaatst 27 juni 2010
- Operatie: aantal artikelen over operatie technieken en gevolgen van operatieve ingrepen bij borstkanker bij elkaar gezet



Plaats een reactie ...
Reageer op "Alleen schildwachtklier verwijderen bij borstkanker geeft na 10 jaar zelfde resultaten op overall overleving en kans op recidief dan volledige okselklierdissectie"