27 september 2015: Bron: PLoS One. 2015 Jun 18;10(6):e0130142. doi: 10.1371/journal.pone.0130142. eCollection 2015.
De laatste jaren vindt er een enorme ontwikkeling plaats met zogeheten anti-PD medicijnen (anti programmed death) ook wel checkpoint remmers genoemd, die ingezet worden als immuuntherapeutische aanpak, zoals de bekendste nivolumab, Pembrolizumab en atezolimab voorheen MPDL3280A geheten. Maar er zijn veel meer anti-PD medicijnen in studies actief. Ik denk persoonlijk dat met deze anti-PD medicijnen een heleboel kanker onder controle kan worden gebracht omdat het werkt als een vorm van immuuntherapie waarbij het apoptose mechanisme (zelfdoding van de cel) wordt hersteld. Waardoor beschadigde cellen of cellen die hun werk hebben gedaan op een natuurlijke manier worden opgeruimd.
Ialiaanse onderzoekers hebben onderzocht of er nog verschil zit in effectiviteit en kans van aanslaan van deze medicijnen of een patiënt de zogeheten Ligand-1 receptorenstatus / DNA mutatie heeft.
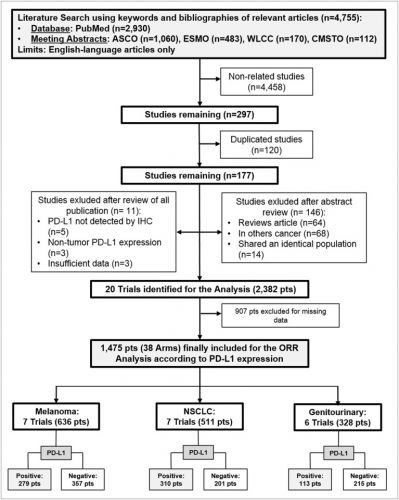
Hieronder de grafiek welke studies bij welke vorm van kanker zij de data hebben verzameld. In dit geval bij melanomen, longkanker en spijsverteringskanker omdat daarin het meest bekend is van studies, maar anti-PD medicijnen werken in principe bij alle vormen van kanker met solide tumoren.
Zij ontdekten dat er wel enig verschil in zit in de kans van succes maar ook kankerpatiënten zonder de Ligand-1 receptorstatus reageren vaak goed op anti-PD medicijnen. Het is ook goed te weten dat deze anti-PD medicijnen tot nu toe ingezet worden bij mensen die al eerder meerdere behandelingen hebben gehad. Interessant zou natuurlijk zijn om deze anti-PD medicijnen in te zetten als immuuntherapie na de eerste diagnose.
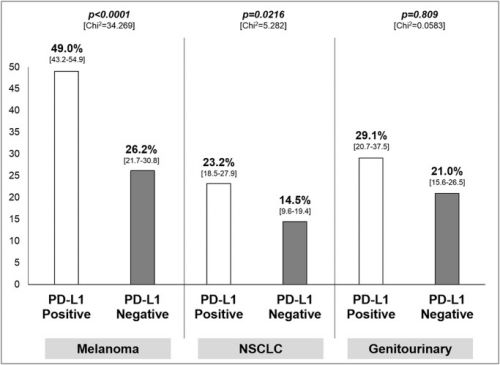
Hier de grafiek van het verschil in Ligand-1 status:
Het is te veel om het studieversalg te vertalen. Zoek in onze zoekmachine op genoemde medicijnen voor studies. Het volledige studierapport: Differential Activity of Nivolumab, Pembrolizumab and MPDL3280A according to the Tumor Expression of Programmed Death-Ligand-1 (PD-L1): Sensitivity Analysis of Trials in Melanoma, Lung and Genitourinary Cancers is gratis in te zien met mooie overzichtsgrafieken en interessante referentielijst van studies met ani-PD medicijnen.
Hier het abstract van de studie:
three antibodies provide a significant differential effThe predictive value of PD-L1 on tumor cells seems to be more robust for anti-PD-1 antibody (nivolumab and pembrolizumab), and in the context of advanced melanoma and NSCLC
Differential Activity of Nivolumab, Pembrolizumab and MPDL3280A according to the Tumor Expression of Programmed Death-Ligand-1 (PD-L1): Sensitivity Analysis of Trials in Melanoma, Lung and Genitourinary Cancers.
Author information
- 1Medical Oncology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy.
- 2Medical Oncology, Regina Elena National Cancer Institute, Roma, Italy.
- 3Department of Pathology and Diagnostic, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy.
- 4Agenzia Italiana del Farmaco (AIFA), Roma, Italy.
- 5Biostatistics, Regina Elena National Cancer Institute, Roma, Italy.
- 6Department of Pathology and Diagnostic, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy; ARC-NET Center for Applied Research on Cancer, Verona, Italy.
Abstract
BACKGROUND:
The potential predictive role of programmed death-ligand-1 (PD-L1) expression on tumor cells in the context of solid tumor treated with checkpoint inhibitors targeting the PD-1 pathway represents an issue for clinical research.
METHODS:
Overall response rate (ORR) was extracted from phase I-III trials investigating nivolumab, pembrolizumab and MPDL3280A for advanced melanoma, non-small cell lung cancer (NSCLC) and genitourinary cancer, and cumulated by adopting a fixed and random-effect model with 95% confidence interval (CI). Interaction test according to tumor PD-L1 was accomplished. A sensitivity analysis according to adopted drug, tumor type, PD-L1 cut-off and treatment line was performed.
RESULTS:
Twenty trials (1,475 patients) were identified. A significant interaction (p<0.0001) according to tumor PD-L1 expression was found in the overall sample with an ORR of 34.1% (95% CI 27.6-41.3%) in the PD-L1 positive and 19.9% (95% CI 15.4-25.3%) in the PD-L1 negative population. ORR was significantly higher in PD-L1 positive in comparison to PD-L1 negative patients for nivolumab and pembrolizumab, with an absolute difference of 16.4% and 19.5%, respectively. A significant difference in activity of 22.8% and 8.7% according to PD-L1 was found for melanoma and NSCLC, respectively, with no significant difference for genitourinary cancer.
CONCLUSION:
Overall, the three antibodies provide a significant differential effect in terms of activity according to PD-L1 expression on tumor cells. The predictive value of PD-L1 on tumor cells seems to be more robust for anti-PD-1 antibody (nivolumab and pembrolizumab), and in the context of advanced melanoma and NSCLC.
- PMID:
- 26086854
- [PubMed - in process]
- PMCID:
- PMC4472786
-
References
1. Dong H, Strome SE, Salomao DR, Tamura H, Hirano F, Flies DB, et al. Tumor-associated B7-H1 promotes T-cell apoptosis: a potential mechanism of immune evasion. Nat Med. 2002;8(8):793–800. [PubMed]2. Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science. 1996;271(5256):1734–6. [PubMed]3. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252–64. doi: 10.1038/nrc3239 [PubMed]4. Topalian SL, Drake CG, Pardoll DM. Immune Checkpoint Blockade: A Common Denominator Approach to Cancer Therapy. Cancer cell. 2015;27(4):450–61. doi: 10.1016/j.ccell.2015.03.001 [PMC free article] [PubMed]5. Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23. doi: 10.1056/NEJMoa1003466 [PMC free article] [PubMed]6. Ribas A. Tumor immunotherapy directed at PD-1. N Engl J Med. 2012;366(26):2517–9. doi: 10.1056/NEJMe1205943 [PubMed]7. Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54. doi: 10.1056/NEJMoa1200690 [PMC free article] [PubMed]8. Postow MA, Callahan MK, Wolchok JD. Immune Checkpoint Blockade in Cancer Therapy. J Clin Oncol. 2015. [Epub ahead of print] [PubMed]9. Robert C, Ribas A, Wolchok JD, Hodi FS, Hamid O, Kefford R, et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet. 2014;384(9948):1109–17. doi: 10.1016/S0140-6736(14)60958-2 [PubMed]10. Weber JS, D'Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16(4):375–84. doi: 10.1016/S1470-2045(15)70076-8 [PubMed]11. Rizvi NA, Mazieres J, Planchard D, Stinchcombe TE, Dy GK, Antonia SJ, et al. Activity and safety of nivolumab, an anti-PD-1 immune checkpoint inhibitor, for patients with advanced, refractory squamous non-small-cell lung cancer (CheckMate 063): a phase 2, single-arm trial. Lancet Oncol. 2015;16(3):257–65. doi: 10.1016/S1470-2045(15)70054-9 [PubMed]12. Armand P, Nagler A, Weller EA, Devine SM, Avigan DE, Chen YB, et al. Disabling immune tolerance by programmed death-1 blockade with pidilizumab after autologous hematopoietic stem-cell transplantation for diffuse large B-cell lymphoma: results of an international phase II trial. J Clin Oncol. 2013;31(33):4199–206. doi: 10.1200/JCO.2012.48.3685 [PubMed]13. Westin JR, Chu F, Zhang M, Fayad LE, Kwak LW, Fowler N, et al. Safety and activity of PD1 blockade by pidilizumab in combination with rituximab in patients with relapsed follicular lymphoma: a single group, open-label, phase 2 trial. Lancet Oncol. 2014;15(1):69–77. doi: 10.1016/S1470-2045(13)70551-5 [PMC free article] [PubMed]14. Motzer RJ, Rini BI, McDermott DF, Redman BG, Kuzel TM, Harrison MR, et al. Nivolumab for Metastatic Renal Cell Carcinoma: Results of a Randomized Phase II Trial. J Clin Oncol. 2014;33(13):1430–7 doi: 10.1200/JCO.2014.59.0703 [PubMed]15. Powles T, Eder JP, Fine GD, Braiteh FS, Loriot Y, Cruz C, et al. MPDL3280A (anti-PD-L1) treatment leads to clinical activity in metastatic bladder cancer. Nature. 2014;515(7528):558–62. doi: 10.1038/nature13904 [PubMed]16. Brahmer JR, Tykodi SS, Chow LQ, Hwu WJ, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366(26):2455–65. doi: 10.1056/NEJMoa1200694 [PMC free article] [PubMed]17. Hamid O, Robert C, Daud A, Hodi FS, Hwu WJ, Kefford R, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369(2):134–44. doi: 10.1056/NEJMoa1305133 [PMC free article] [PubMed]18. Topalian SL, Sznol M, McDermott DF, Kluger HM, Carvajal RD, Sharfman WH, et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J Clin Oncol. 2014;32(10):1020–30. doi: 10.1200/JCO.2013.53.0105 [PubMed]19. Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122–33. doi: 10.1056/NEJMoa1302369 [PubMed]20. Mahoney KM, Atkins MB. Prognostic and predictive markers for the new immunotherapies. Oncology. 2014;28 Suppl 3:39–48. [PubMed]21. Gadiot J, Hooijkaas AI, Kaiser AD, van Tinteren H, van Boven H, Blank C. Overall survival and PD-L1 expression in metastasized malignant melanoma. Cancer. 2011;117(10):2192–201. doi: 10.1002/cncr.25747 [PubMed]22. Thompson RH, Kuntz SM, Leibovich BC, Dong H, Lohse CM, Webster WS, et al. Tumor B7-H1 is associated with poor prognosis in renal cell carcinoma patients with long-term follow-up. Cancer Res. 2006;66(7):3381–5. [PubMed]23. Wang A, Wang HY, Liu Y, Zhao MC, Zhang HJ, Lu ZY, et al. The prognostic value of PD-L1 expression for non-small cell lung cancer patients: A meta-analysis. Eur J Sur Oncol. 2015;41(4):450–456 [PubMed]24. Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372(4):320–30. doi: 10.1056/NEJMoa1412082 [PubMed]25. Pignon JP, Hill C. Meta-analyses of randomised clinical trials in oncology. Lancet Oncol. 2001;2(8):475–82. [PubMed]26. Bria E, Gralla RJ, Raftopoulos H, Cuppone F, Milella M, Sperduti I, et al. Magnitude of benefit of adjuvant chemotherapy for non-small cell lung cancer: Meta-analysis of randomized clinical trials. Lung Cancer. 2009;63(1):50–7. doi: 10.1016/j.lungcan.2008.05.002 [PubMed]27. Higgins JPT, Green S. Cochrane handbook for Systematic Reviews of intervention 4.2.6 [updated sep 2006] The Cochrane Library. Issue 4 Chichester, UK: John Wiley & Sons, Ltd; 2006.28. Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–34. [PubMed]29. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16 [PMC free article] [PubMed]30. Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219 [PMC free article] [PubMed]31. Pilotto S, Di Maio M, Peretti U, Kinspergher S, Brunelli M, Massari F, et al. Predictors of outcome for patients with lung adenocarcinoma carrying the epidermal growth factor receptor mutation receiving 1st-line tyrosine kinase inhibitors: Sensitivity and meta-regression analysis of randomized trials. Crit Rev Oncol Hematol. 2014;90(2):135–45. doi: 10.1016/j.critrevonc.2013.11.005 [PubMed]32. Choueiri T, Fishman MN, Escudier B, Kim JJ, Kluger H, Stadler WM, et al. 1051PDImmunomodulatory activity of nivolumab in previously treated and untreated metastatic renal cell carcinoma (MRCC): biomarker-based results from a randomized clinical trial. Ann Oncol. 2014;25(suppl 4):iv362.33. Hamid O, Sosman JA, Lawrence DP, Sullivan RJ, Ibrahim N, Kluger HM, et al. Clinical activity, safety, and biomarkers of MPDL3280A, an engineered PD-L1 antibody in patients with locally advanced or metastatic melanoma (mM). ASCO Meeting Abstracts. 2013;31(15_suppl):9010.34. Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515(7528):563–7. doi: 10.1038/nature14011 [PubMed]35. Hodi FS, Sznol M, Kluger HM, McDermott DF, Carvajal RD, Lawrence DP, et al. Long-term survival of ipilimumab-naive patients (pts) with advanced melanoma (MEL) treated with nivolumab (anti-PD-1, BMS-936558, ONO-4538) in a phase I trial. ASCO Meeting Abstracts. 2014;32(15_suppl):9002.36. Kefford R, Ribas A, Hamid O, Robert C, Daud A, Wolchok JD, et al. Clinical efficacy and correlation with tumor PD-L1 expression in patients (pts) with melanoma (MEL) treated with the anti-PD-1 monoclonal antibody MK-3475. ASCO Meeting Abstracts. 2014;32(15_suppl):3005.37. Rizvi NA, Garon EB, Patnaik A, Gandhi L, Leighl NB, Balmanoukian AS, et al. Safety and clinical activity of MK-3475 as initial therapy in patients with advanced non-small cell lung cancer (NSCLC). ASCO Meeting Abstracts. 2014;32(15_suppl):8007.38. Sznol M, Kluger HM, Callahan MK, Postow MA, Gordon RA, Segal NH, et al. Survival, response duration, and activity by BRAF mutation (MT) status of nivolumab (NIVO, anti-PD-1, BMS-936558, ONO-4538) and ipilimumab (IPI) concurrent therapy in advanced melanoma (MEL). ASCO Meeting Abstracts. 2014;32(15_suppl):LBA9003.39. Weber JS, Kudchadkar RR, Yu B, Gallenstein D, Horak CE, Inzunza HD, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab-refractory or -naive melanoma. J Clin Oncol. 2013;31(34):4311–8. doi: 10.1200/JCO.2013.51.4802 [PMC free article] [PubMed]40. Hammers H, Plimack ER, Infante JR, Ernstoff M, Rini BI, McDermott DF, et al. 1050OPhase I study of nivolumab in combination with ipilimumab in metastatic renal cell carcinoma (MRCC). Ann Oncol. 2014;25(suppl 4):iv361–iv2.41. Plimack ER, Gupta S, Bellmunt J, Berger R, Montgomery B, Gonzalez EJ, et al. LBA23A Phase 1B study of pembrolizumab (pembro; mk-3475) in patients (pts) with advanced urothelial tract cancer. Ann Oncol. 2014;25(suppl 4).42. Cho DC, Sosman JA, Sznol M, Gordon MS, Hollebecque A, Hamid O, et al. Clinical activity, safety, and biomarkers of MPDL3280A, an engineered PD-L1 antibody in patients with metastatic renal cell carcinoma (mRCC). ASCO Meeting Abstracts. 2013;31(15_suppl):4505.43. Rizvi NA, Shepherd FA, Antonia SJ, Brahmer JR, Chow LQ, Goldman J, et al. First-Line Monotherapy With Nivolumab (Anti-PD-1; BMS-936558, ONO-4538) in Advanced Non-Small Cell Lung Cancer (NSCLC): Safety, Efficacy, and Correlation of Outcomes With PD-L1 Status. Int J Radiation Oncol Biol Phys. 2014;90(5):S31.44. Antonia SJ, Gettinger S, Goldman J, Chow LQ, Juergens R, Borghaei H, et al. Safety and Efficacy of First-Line Nivolumab (Anti-PD-1; BMS-936558, ONO-4538) and Ipilimumab in Non-Small Cell Lung Cancer (NSCLC). Int J Radiation Oncol Biol Phys. 2014;90(5):S32–S3.45. Gettinger SN, Horn L, Gandhi L, Spigel DR, Antonia SJ, Rizvi NA, et al. Overall Survival and Long-Term Safety of Nivolumab (Anti-Programmed Death 1 Antibody, BMS-936558, ONO-4538) in Patients With Previously Treated Advanced Non-Small-Cell Lung Cancer. J Clin Oncol. 2015. [Epub ahead of print] [PubMed]46. Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the Treatment of Non-Small-Cell Lung Cancer. N Engl J Med. 2015. [Epub ahead of print] [PubMed]47. Patel SP, Kurzrock R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol Cancer Ther. 2015;14(4):847–56. [PubMed]48. Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med. 2015. [Epub ahead of print] [PubMed]49. Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515(7528):568–71. doi: 10.1038/nature13954 [PMC free article] [PubMed]50. Taube JM, Klein A, Brahmer JR, Xu H, Pan X, Kim JH, et al. Association of PD-1, PD-1 ligands, and other features of the tumor immune microenvironment with response to anti-PD-1 therapy. Clin Cancer Res. 2014;20(19):5064–74. doi: 10.1158/1078-0432.CCR-13-3271 [PMC free article] [PubMed]51. Gubin MM, Zhang X, Schuster H, Caron E, Ward JP, Noguchi T, et al. Checkpoint blockade cancer immunotherapy targets tumour-specific mutant antigens. Nature. 2014;515(7528):577–81. doi: 10.1038/nature13988 [PMC free article] [PubMed]52. Wolchok JD, Chan TA. Cancer: Antitumour immunity gets a boost. Nature. 2014;515(7528):496–8. doi: 10.1038/515496a [PubMed]53. Yadav M, Jhunjhunwala S, Phung QT, Lupardus P, Tanguay J, Bumbaca S, et al. Predicting immunogenic tumour mutations by combining mass spectrometry and exome sequencing. Nature. 2014;515(7528):572–6. doi: 10.1038/nature14001 [PubMed]54. Boussiotis VA. Somatic mutations and immunotherapy outcome with CTLA-4 blockade in melanoma. N Engl J Med. 2014;371(23):2230–2. doi: 10.1056/NEJMe1413061 [PMC free article] [PubMed]55. Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. The New England journal of medicine. 2014;371(23):2189–99. doi: 10.1056/NEJMoa1406498 [PMC free article] [PubMed]56. Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348(6230):124–8. doi: 10.1126/science.aaa1348 [PubMed]57. Postow MA, Chesney J, Pavlick AC, Robert C, Grossmann K, McDermott D, et al. Nivolumab and Ipilimumab versus Ipilimumab in Untreated Melanoma. N Engl J Med. 2015. [Epub ahead of print] [PubMed]
Articles from PLoS ONE are provided here courtesy of Public Library of Science
Gerelateerde artikelen
- CRISPR-Cas9 bewerkte T-cellen gericht op het intracellulaire immuuncontrolepunt CISH maakt patienten met gevorderde darmkanker alsnog gevoelig voor immuuntherapie met anti-PD medicijnen waar deze eerder ongevoelig voor waren of resistentie lieten zien. co
- DCVax-direct = immuuntherapie met dendritische cellen geeft hoopvolle resultaten bij 13 verschillende vormen van kanker met solide tumoren
- Solide tumoren: CRISPR-Cas9 gentherapie gericht op afwijkende DNA mutaties en gecombineerd met gemoduleerde T-cellen geeft hoopvolle resultaten bij drie patienten met vergevorderde kanker.
- Solide tumoren: Metronomische chemotherapie = dagelijks lage doses chemo naast immuuntherapie met nivolumab verbetert effectiviteit bij vormen van kanker met solide tumoren bij kinderen
- Solide tumoren: Tisotumab vedotin plus chemo geeft spectaculaire resultaten bij zwaarvoorbehandelde kankerpatienten met verschillende primaire vormen van kanker met solide tumoren.
- Solide tumoren: Interleukine-2 (IL-2) hoge dosis in medicijnproducerende bolletjes via kleine operatie ingebracht geneest muizen met gevorderde darmkanker en eierstokkanker binnen 6 dagen.
- Solide tumoren: Vesicular stomatitis virus (VSV-GP) een gemoduleerd oncolytisch virus geeft in combinatie met anti-PD medicijn ezabenlimab bij kankerpatienten met solide tumoren hoopvolle eerste resultaten
- Solide tumoren: Apceden, een gepersonaliseerd vaccin toegevoegd aan dendritische celtherapie geeft opvallend goede resultaten bij solide tumoren, waaronder ook prostaatkanker
- Solide tumoren: Hoge tumormutatiebelasting (TMB) als biomarker en prognose voor behandeling met immuuntherapie met anti-PD medicijnen is niet veel beter in uiteindelijk resultaat dan lage tumormutatiebelasting
- Solide tumoren: Lenvatinib + Pembrolizumab bij patiënten met inoperabele gevorderde nierkanker, baarmoederkanker, melanomen en andere gevorderde kanker met solide tumoren geeft uitstekende resultaten met meer dan de helft remissies van 50 procent of meer
- Solide tumoren: Vaccin tegen KRAS positief gemuteerde vormen van kanker - darmkankers en longkanker o.a. - wordt gecombineerd met trametinib een anti-PD medicijn in fase I studie na hoopvolle resultaten. copy 1
- Solide tumoren: pembrolizumab bij patiënten met vormen van uitgezaaide kanker, anders dan darmkanker, met hoge microsatellietinstabiliteit (MSI-H) en DNA-mismatch-reparatie-deficiënte (dMMR) geeft uitstekende en duurzame resultaten op overall overleving
- Solide tumoren: PD-L1 - blokkade met monoklonale anti lichamen - een vorm van immuuntherapie - zorgt bij verschillende vormen van kanker voor opmerkelijke resultaten
- Solide tumoren: Immuuntherapie op de PD-L1 expressie gericht met een zogeheten humaan monoklonaal antilichaam bekend onder de naam MPDL3280A zorgt al voor opmerkelijke resultaten in een fase I studie bij patiënten met solide tumoren
- Solide tumoren: Immuuntherapie met ipilimumab na gerichte stereotactische bestraling geeft uitstekende resultaten bij 26 ot 57 procent van100 zwaar voorbehandelde patienten met vergevorderde in lever en longen uitgezaaide kanker met solide tumoren
- Solide tumoren: Immuuntherapie alleen in vergelijking met immuuntherapie samen met chemotherapie bij kankerpatienten met solide tumoren geeft betere resultaten bij mannen dan bij vrouwen blijkt uit grote reviewstudie van 16 gerandomiseerde studies
- Solide tumoren: Immuuntherapie bij urologische vormen van kanker, blaaskanker, prostaatkanker en nierkanker is veelbelovend. Recente studies bewijzen langdurige remissies
- Solide tumoren: HPS - heat shock protein zorgt voor opmerkelijke resultaten bij allerlei vormen van kanker met solide tumoren. Vooral bij longkanker en darmkanker
- Solide tumoren: Immuuntherapie met nivolumab zorgt voor duurzame en sterk verbeterde overall overleving bij verschillende vormen van kanker, melanomen, longkanker en nierkanker
- Solide tumoren: Anti-PD medicijnen zoals nivolumab, Pembrolizumab en atezolizumab gegeven als immuuntherapie geven zeer goede resultaten bij verschillende vormen van kanker met solide tumoren, zelfs zonder Ligand-1 receptorstatus
- Solide tumoren: Vaccin gebaseerd op specifiek eiwit verbonden aan p53 gen en inspuiten van lichaamseigene dendritische cellen geeft veelbelovende resultaten in dierproeven bij niet-klein-cellige longkanker en borstkanker en hoofd en halstumoren.
- Solide tumoren: Kankerpatienten met solide tumoren met MSI-H = hoge microsatelliet instabiliteit en mismatch reparatie (dMMR) reageren uitstekend op immuuntherapie met pembrolizumab vooraf aan operatie met 65 tot 80 procent complete remissies



Plaats een reactie ...
Reageer op "Solide tumoren: Anti-PD medicijnen zoals nivolumab, Pembrolizumab en atezolizumab gegeven als immuuntherapie geven zeer goede resultaten bij verschillende vormen van kanker met solide tumoren, zelfs zonder Ligand-1 receptorstatus"