Uit Amerikaans epidemologisch onderzoek van 2005 tot 2018 naar relatie tussen PFAS (Poly- en perfluoralkylstoffen) en kanker op basis van datagegevens bij volwassenen vanaf 20 jaar uit het National Health and Nutrition Examination Survey (NHANES) blijkt dat vrouwen die veel blootgesteld waren aan bepaalde PFAS bevattende producten, gediagnosticeerd werden met vooral hormoon gerelateerde vormen van kanker, waaronder eierstokkanker maar ook vaker een diagnose hadden van melanomen. Bij mannen werden geen of nauwelijks verschillen ontdekt in diagnoses van kanker gerelateerd aan PFAS bevattende producten.
PFAS (Poly- en perfluoralkylstoffen) bevattende producten worden gebruikt in duizenden huishoudelijke en industriële producten. Pfas is een verzamelnaam voor duizenden chemische stoffen die van nature niet in het milieu voorkomen. De afkorting PFAS staat voor poly- en perfluoralkylstoffen. Er zijn ongeveer 5000 verschillende soorten pfas. De bekendste voorbeelden zijn GenX, PFOA en PFOS. De stoffen zijn geliefd in de industrie omdat ze hittebestendig en vocht-, vet- en vuilafstotend zijn. Ze worden gebruikt in producten als pannen, waterafstotende kleding, blusschuim en cosmetica. De stoffen zijn slecht voor het milieu, nauwelijks afbreekbaar en schadelijk voor het afweersysteem. Een aantal types zijn bij langdurige blootstelling kankerverwekkend.
PFAS was en is in het nieuws door Chemour en 3FM en de Westerschelde.
In het abstract staat o.a.: "Biomarkers in alle blootstellingscategorieën (fenolen, parabenen en per- en polyfluoralkylstoffen) werden cross-sectioneel geassocieerd met een verhoogde kans op eerdere melanoomdiagnoses bij vrouwen, en een verhoogde kans op eerdere eierstokkanker werd geassocieerd met verschillende fenolen en parabenen."
Het onderzoek omvatte voor PFAS 16.696 vrouwen en mannen. Voor Fenolen 10.428 mannen en vrouwen. Zie onderstaande grafiek: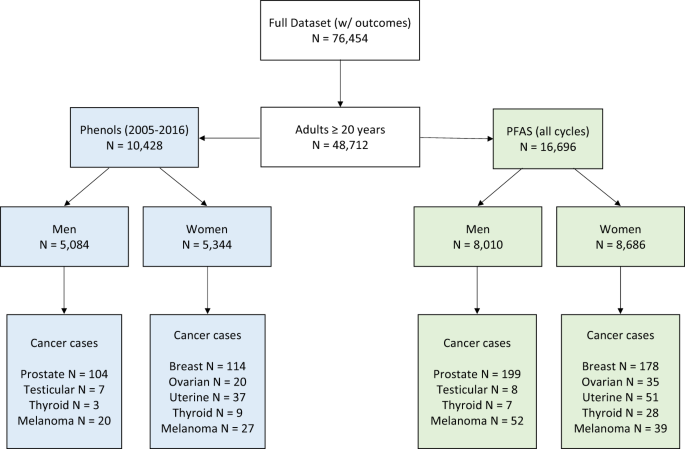
Het Algemeen Dagblad heeft een uitgebreid artikel erover:
Studie koppelt blootstelling aan PFAS-chemicaliën aan hogere kans op kanker bij vrouwen
Het volledige studierapport is gratis in te zien of te downloaden:
- Article
- Open Access
- Published:
Exploratory profiles of phenols, parabens, and per- and poly-fluoroalkyl substances among NHANES study participants in association with previous cancer diagnoses
Journal of Exposure Science & Environmental Epidemiology (2023)
Abstract
Background
Some hormonally active cancers have low survival rates, but a large proportion of their incidence remains unexplained. Endocrine disrupting chemicals may affect hormone pathways in the pathology of these cancers.
Objective
To evaluate cross-sectional associations between per- and polyfluoroalkyl substances (PFAS), phenols, and parabens and self-reported previous cancer diagnoses in the National Health and Nutrition Examination Survey (NHANES).
Methods
We extracted concentrations of 7 PFAS and 12 phenols/parabens and self-reported diagnoses of melanoma and cancers of the thyroid, breast, ovary, uterus, and prostate in men and women (≥20 years). Associations between previous cancer diagnoses and an interquartile range increase in exposure biomarkers were evaluated using logistic regression models adjusted for key covariates. We conceptualized race as social construct proxy of structural social factors and examined associations in non-Hispanic Black, Mexican American, and other Hispanic participants separately compared to White participants.
Results
Previous melanoma in women was associated with higher PFDE (OR:2.07, 95% CI: 1.25, 3.43), PFNA (OR:1.72, 95% CI: 1.09, 2.73), PFUA (OR:1.76, 95% CI: 1.07, 2.89), BP3 (OR: 1.81, 95% CI: 1.10, 2.96), DCP25 (OR: 2.41, 95% CI: 1.22, 4.76), and DCP24 (OR: 1.85, 95% CI: 1.05, 3.26). Previous ovarian cancer was associated with higher DCP25 (OR: 2.80, 95% CI: 1.08, 7.27), BPA (OR: 1.93, 95% CI: 1.11, 3.35) and BP3 (OR: 1.76, 95% CI: 1.00, 3.09). Previous uterine cancer was associated with increased PFNA (OR: 1.55, 95% CI: 1.03, 2.34), while higher ethyl paraben was inversely associated (OR: 0.31, 95% CI: 0.12, 0.85). Various PFAS were associated with previous ovarian and uterine cancers in White women, while MPAH or BPF was associated with previous breast cancer among non-White women.
Impact Statement
Biomarkers across all exposure categories (phenols, parabens, and per- and poly- fluoroalkyl substances) were cross-sectionally associated with increased odds of previous melanoma diagnoses in women, and increased odds of previous ovarian cancer was associated with several phenols and parabens. Some associations differed by racial group, which is particularly impactful given the established racial disparities in distributions of exposure to these chemicals. This is the first epidemiological study to investigate exposure to phenols in relation to previous cancer diagnoses, and the first NHANES study to explore racial/ethnic disparities in associations between environmental phenol, paraben, and PFAS exposures and historical cancer diagnosis.
Data availability
NHANES data is publicly available. The analytical dataset for this study and code can be available upon request (Amber Cathey [acathey@umich.edu], Max Aung [maxaung@usc.edu]).
References
-
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7–34.
-
Sutton P, Kavanaugh-Lynch MHE, Plumb M, Yen IH, Sarantis H, Thomsen CL, et al. California Breast Cancer Prevention Initiatives: Setting a research agenda for prevention. Reprod Toxicol. 2015;54:11–18.
-
Aul P, Ichtenstein L, Olm IVH, Erkasalo IKV, Nastasia A, Liadou I, et al. Environmental and heritable factors in the causation of cancer analyses of cohorts of twins from Sweden, Denmark, and Finland. N. Engl J Med. 2000;343:78–85.
-
Risbridger GP, Davis ID, Birrell SN, Tilley WD. Breast and prostate cancer: more similar than different. Nat Rev Cancer. 2010;10:205–12.
-
Kiyama R, Wada-Kiyama Y. Estrogenic endocrine disruptors: Molecular mechanisms of action. Environ Int. 2015;83:11–40.
-
Aker AM, Ferguson KK, Rosario ZY, Mukherjee B, Alshawabkeh AN, Calafat AM, et al. A repeated measures study of phenol, paraben and Triclocarban urinary biomarkers and circulating maternal hormones during gestation in the Puerto Rico PROTECT cohort. Environ Health. 2019;18:28.
-
Aung MT, Johns LE, Ferguson KK, Mukherjee B, McElrath TF, Meeker JD. Thyroid hormone parameters during pregnancy in relation to urinary bisphenol A concentrations: A repeated measures study. Environ Int. 2017;104:33–40.
-
Ballesteros V, Costa O, Iñiguez C, Fletcher T, Ballester F, Lopez-Espinosa M-J. Exposure to perfluoroalkyl substances and thyroid function in pregnant women and children: A systematic review of epidemiologic studies. Environ Int. 2017;99:15–28.
-
Wang Y, Aimuzi R, Nian M, Zhang Y, Luo K, Zhang J. Perfluoroalkyl substances and sex hormones in postmenopausal women: NHANES 2013-2016. Environ Int. 2021;149:106408.
-
Smith MT, Guyton KZ, Gibbons CF, Fritz JM, Portier CJ, Rusyn I, et al. Key characteristics of carcinogens as a basis for organizing data on mechanisms of carcinogenesis. Environ Health Perspect. 2016;124:713.
-
Hafezi SA, Abdel-Rahman WM. The endocrine disruptor bisphenol A (BPA) exerts a wide range of effects in carcinogenesis and response to therapy. Curr Mol Pharm. 2019;12:230–8.
-
Bonefeld-Jorgensen EC, Long M, Bossi R, Ayotte P, Asmund G, Krüger T, et al. Perfluorinated compounds are related to breast cancer risk in Greenlandic Inuit: a case control study. Environ Health. 2011;10:88.
-
Bonefeld-Jørgensen EC, Long M, Fredslund SO, Bossi R, Olsen J. Breast cancer risk after exposure to perfluorinated compounds in Danish women: a case-control study nested in the Danish National Birth Cohort. Cancer Causes Control. 2014;25:1439–48.
-
Tsai M-S, Chang S-H, Kuo W-H, Kuo C-H, Li S-Y, Wang M-Y, et al. A case-control study of perfluoroalkyl substances and the risk of breast cancer in Taiwanese women. Environ Int. 2020;142:105850.
-
Mancini FR, Cano-Sancho G, Gambaretti J, Marchand P, Boutron-Ruault M-C, Severi G, et al. Perfluorinated alkylated substances serum concentration and breast cancer risk: Evidence from a nested case-control study in the French E3N cohort. Int J Cancer. 2020;146:917–28.
-
Nguyen VK, Kahana A, Heidt J, Polemi K, Kvasnicka J, Jolliet O, et al. A comprehensive analysis of racial disparities in chemical biomarker concentrations in United States women, 1999–2014. Environ Int. 2020;137:105496.
-
Patel AV, Deubler E, Teras LR, Colditz GA, Lichtman CJ, Cance WG, et al. Key risk factors for the relative and absolute 5-year risk of cancer to enhance cancer screening and prevention. Cancer. 2022;128:3502–15.
-
Calafat AM, Wong LY, Ye X, Reidy JA, Needham LL. Concentrations of the sunscreen agent benzophenone-3 in residents of the United States: National Health and Nutrition Examination Survey 2003–2004. Environ Health Perspect. 2008;116:893.
-
Saginala K, Barsouk A, Aluru JS, Rawla P, Barsouk A. Epidemiology of melanoma. Medical Sciences. 2021;9. https://doi.org/10.3390/MEDSCI9040063.
-
Dawes SM, Tsai S, Gittleman H, Barnholtz-Sloan JS, Bordeaux JS. Racial disparities in melanoma survival. J Am Acad Dermatol. 2016;75:983–91.
-
Barry V, Winquist A, Steenland K. Perfluorooctanoic acid (PFOA) exposures and incident cancers among adults living near a chemical plant. Environ Health Perspect. 2013;121:1313–8.
-
Vieira VM, Hoffman K, Shin H-M, Weinberg JM, Webster TF, Fletcher T. Perfluorooctanoic acid exposure and cancer outcomes in a contaminated community: a geographic analysis. Environ Health Perspect. 2013;121:318–23.
-
Grice MM, Alexander BH, Hoffbeck R, Kampa DM. Self-reported medical conditions in perfluorooctanesulfonyl fluoride manufacturing workers. J Occup Environ Med. 2007;49:722–9.
-
Leonard RC, Kreckmann KH, Sakr CJ, Symons JM. Retrospective cohort mortality study of workers in a polymer production plant including a reference population of regional workers. Ann Epidemiol. 2008;18:15–22.
-
Alexander BH, Olsen GW, Burris JM, Mandel JH, Mandel JS. Mortality of employees of a perfluorooctanesulphonyl fluoride manufacturing facility. Occup Environ Med. 2003;60:722–9.
-
Olsen GW, Burlew MM, Marshall JC, Burris JM, Mandel JH. Analysis of episodes of care in a perfluorooctanesulfonyl fluoride production facility. J Occup Environ Med. 2004;46:837–46.
-
Enninga EAL, Holtan SG, Creedon DJ, Dronca RS, Nevala WK, Ognjanovic S, et al. Immunomodulatory effects of sex hormones: requirements for pregnancy and relevance in melanoma. Mayo Clin Proc. 2014;89:520–35.
-
Nosrati A, Wei ML. Sex disparities in melanoma outcomes: The role of biology. Arch Biochem Biophys. 2014;563:42–50.
-
Walker MJ, Beattie CW, Patel MK, Ronan SM, Das Gupta TK. Estrogen receptor in malignant melanoma. J Clin Oncol. 1987;5:1256–61.
-
Houck KA, Patlewicz G, Richard AM, Williams AJ, Shobair MA, Smeltz M, et al. Bioactivity profiling of per- and polyfluoroalkyl substances (PFAS) identifies potential toxicity pathways related to molecular structure. Toxicology. 2021;457:152789.
-
Li J, Cao H, Feng H, Xue Q, Zhang A, Fu J. Evaluation of the estrogenic/antiestrogenic activities of perfluoroalkyl substances and their interactions with the human estrogen receptor by combining in vitro assays and in silico modeling. Environ Sci Technol. 2020;54:14514–24.
-
Grønnestad R, Johanson SM, Müller MHB, Schlenk D, Tanabe P, Krøkje Å, et al. Effects of an environmentally relevant PFAS mixture on dopamine and steroid hormone levels in exposed mice. Toxicol Appl Pharm. 2021;428:115670.
-
Behr A-C, Lichtenstein D, Braeuning A, Lampen A, Buhrke T. Perfluoroalkylated substances (PFAS) affect neither estrogen and androgen receptor activity nor steroidogenesis in human cells in vitro. Toxicol Lett. 2018;291:51–60.
-
Cronin KA, Scott S, Firth AU, Sung H, Henley SJ, Sherman RL, et al. Annual report to the nation on the status of cancer, part 1: National cancer statistics. Cancer. 2022;128:4251–84.
-
Henley SJ, Miller JW, Dowling NF, Benard VB, Richardson LC. Uterine cancer incidence and mortality — United States, 1999–2016. Morbidity Mortal Wkly Rep. 2018;67:1333.
-
Felix AS, Brinton LA. Cancer progress and priorities: Uterine cancer. Cancer Epidemiol Biomark Prev. 2018;27:985–94.
-
Messmer MF, Salloway J, Shara N, Locwin B, Harvey MW, Traviss N Risk of cancer in a community exposed to per- and poly-fluoroalkyl substances. Environ Health Insights 2022; 16. https://doi.org/10.1177/11786302221076707.
-
Wu NX, Deng LJ, Xiong F, Xie JY, Li XJ, Zeng Q, et al. Risk of thyroid cancer and benign nodules associated with exposure to parabens among Chinese adults in Wuhan, China. Environ Sci Pollut Res Int. 2022;29:70125–34.
-
Doherty JA, Peres LC, Wang C, Way GP, Greene CS, Schildkraut JM. Challenges and opportunities in studying the epidemiology of ovarian cancer subtypes. Curr Epidemiol Rep. 2017;4:211–20.
-
Huffman DL, Jayakrishnan TT, Shankar K, Peterson CE, Wegner RE. Disparities in ovarian cancer treatment and overall survival according to race: An update. Gynecol Oncol. 2021;162:674–8.
-
Reid BM, Permuth JB, Sellers TA. Epidemiology of ovarian cancer: a review. Cancer Biol Med. 2017;14:9–32.
-
Menon U, Karpinskyj C, Gentry-Maharaj A. Ovarian cancer prevention and screening. Obstet Gynecol. 2018;131:909–27.
-
Thiery JP, Sleeman JP. Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–42.
-
Kim Y-S, Hwang K-A, Hyun S-H, Nam K-H, Lee C-K, Choi K-C, et al. and nonylphenol have the potential to stimulate the migration of ovarian cancer cells by inducing epithelial-mesenchymal transition via an estrogen receptor dependent pathway. Chem Res Toxicol. 2015;28:662–71.
-
Ptak A, Hoffmann M, Gruca I, Barć J. Bisphenol A induce ovarian cancer cell migration via the MAPK and PI3K/Akt signalling pathways. Toxicol Lett. 2014;229:357–65.
-
Lau KM, Mok SC, Ho SM. Expression of human estrogen receptor-alpha and -beta, progesterone receptor, and androgen receptor mRNA in normal and malignant ovarian epithelial cells. Proc Natl Acad Sci USA. 1999;96:5722–7.
-
Gao H, Yang B-J, Li N, Feng L-M, Shi X-Y, Zhao W-H, et al. Bisphenol A and hormone-associated cancers: current progress and perspectives. Medicine. 2015;94:e211.
-
Ulm M, Ramesh AV, McNamara KM, Ponnusamy S, Sasano H, Narayanan R. Therapeutic advances in hormone-dependent cancers: focus on prostate, breast, and ovarian cancers. Endocr Connect. 2019;8:R10–R26.
-
Gonzalez TL, Rae JM, Colacino JA. Implication of environmental estrogens on breast cancer treatment and progression. Toxicology. 2019;421:41–48.
-
Dowsett M, Cuzick J, Ingle J, Coates A, Forbes J, Bliss J, et al. Meta-analysis of breast cancer outcomes in adjuvant trials of aromatase inhibitors versus tamoxifen. J Clin Oncol. 2010;28:509–18.
-
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-Year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N. Engl J Med. 2017;377:1836–46.
-
Zota AR, Shamasunder B. The environmental injustice of beauty: framing chemical exposures from beauty products as a health disparities concern. Am J Obstet Gynecol. 2017;217:418.e1–418.e6.
-
Lee S, Kar A, Reade A. Dirty water: Toxic ‘forever’ PFAS chemicals are prevalent in the drinking water of environmental justice communities. https://www.nrdc.org/sites/default/files/dirty-water-pfas-ej-communities-report.pdf (accessed 28 Jun 2023).
-
Henley SJ, Miller JW, Dowling NF, Benard VB, Richardson LC. Uterine cancer incidence and mortality - United States, 1999-2016. MMWR Morb Mortal Wkly Rep. 2018;67:1333–8.
-
Zavala VA, Bracci PM, Carethers JM, Carvajal-Carmona L, Coggins NB, Cruz-Correa MR, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. 2021;124:315–32.
-
Liu Y, Zhou JW, Liu CD, Yang JK, Liao DY, Liang ZJ, et al. Comprehensive signature analysis of drug metabolism differences in the White, Black and Asian prostate cancer patients. Aging. 2021;13:16316–40.
-
Bergmann MM, Calle EE, Mervis CA, Miracle-McMahill HL, Thun MJ, Heath CW. Validity of self-reported cancers in a prospective cohort study in comparison with data from state cancer registries. Am J Epidemiol. 1998;147:556–62.
Acknowledgements
Support for this research was provided by core center grant P30-ES030284 from the National Institute of Environmental Health Sciences and the Helen Diller Family Comprehensive Cancer Center grant 5P30CA082103-23. Support for Drs. Aung, Woodruff, and Reynolds was provided in part by NCI/NIEHS grant 1UG3CA265845-01. Support for Dr. Aung was also partly provided by NIEHS core center grant P30-ES00748. Support for Drs. Colacino and Nguyen were partly provided by NIEHS core center grant P30ES017885 and NIEHS grant R01ES028802. Dr. Colacino was also partly supported by NCI/NIEHS grant UG3CA267907. Dr. Nguyen was partially supported by the Harvard Data Science Initiative.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium.
Author information
Authors and Affiliations
Contributions
ALC: formal analysis, investigation, methodology, visualization, writing - original draft, writing - review and editing; VKN: methodology, writing - review and editing; JAC: supervision, writing - review and editing; TJW: supervision, writing - review and editing; PR: conceptualization, project administration, supervision, writing - review and editing; MTA: conceptualization, funding acquisition, project administration, supervision, writing - review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cathey, A.L., Nguyen, V.K., Colacino, J.A. et al. Exploratory profiles of phenols, parabens, and per- and poly-fluoroalkyl substances among NHANES study participants in association with previous cancer diagnoses. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00601-6
-
Received
-
Revised
-
Accepted
-
Published
-
DOIhttps://doi.org/10.1038/s41370-023-00601-6
Gerelateerde artikelen
- Algemeen: Voeding en voedingstoffen die een preventief effect hebben om kanker: te voorkomen. Een aantal studies en aanbevelingen bij elkaar gezet.
- ALS - amyotrofische laterale sclerose is via een bloedtest 10 jaar eerder te ontdekken voordat symptomen tot klachten gaan leiden
- Alzheimer - dementie is via een bloedtest jaren voordat de ziekte zich openbaart op te sporen en daardoor wellicht ook te voorkomen of uit te stellen voordat de ziekte ernstig wordt.
- Antibiotica speelt mogelijk rol bij ontstaan PDS - Prikkelbare Darm Syndroom.
- Asbest lijkt ook kanker in het strottenhoofd, maagkanker en darmkanker te kunnen veroorzaken.
- Aspirine ter voorkoming van kanker of een recidief van kanker: een overzicht van studies met aspirine copy 1
- Bacterien in de mond - Commensale microbiome en met name Genera Corynebacterium en Kingela spelen grote rol in wel of niet ontwikkelen van mond- en keelkanker. Vooral bij zware rokers en drinkers.
- Diakonessenhuis Utrecht biedt VEGA-Checker aan die bloedwaarden controleert of je lichaam wel alle vitamines en mineralen binnenkrijgt die het nodig heeft.
- DIM - diindolylmethane voorkomt voor 100 procent baarmoederhalskanker (100 procent vs 61 procent bij placebo) bij vrouwen met hoog risico door aanwezigheid van intraepithelial neoplasia (CIN I–II)
- Bloedbiomarker waarden van CRP, LDL cholesterol en lipoproteïne (a), kunnen vrouwen tientallen jaren van tevoren een beeld geven van hun risico op hartziekten
- Bloedtest die methyl meet in cellen kan ruim van te voren voorspellen of iemand borstkanker gaat ontwikkelen. Blijkt uit jarenlang onderzoek. copy 1
- Baarmoederhalskanker veel beter - 60 procent - te voorkomen door DNA test op het HPV virus in vergelijking met uitstrijkje
- Baarmoederkanker is te voorkomen (tot 40 procent) met veel bewegen en stabiel lichaamsgewicht. Te dik geeft meer risico op baarmoederkanker.
- Bewegen: Mensen die te weinig bewegen en zittend hun dagen doorbrengen hadden 82 procent hoger risico om te overlijden aan kanker vergeleken met mensen die veel bewegen en sporten, zelfs na correctie voor leeftijd, geslacht en ziektestatus.
- Bovine Lactoferrin (bLF) stimuleert het immuunsysteem en remt groei darmpoliepen, aldus dubbelblinde gerandomiseerde studie.
- Borstkanker - preventie: een overzicht van belangrijke artikelen en recente studies hoe het risico op borstkanker te verkleinen
- BRCA-1 mutatie verdubbelt risico op baarmoederkanker bij vrouwen met BRCA-1 gen en 26x grotere kans in vergelijking met vrouwen zonder BRCA mutaties
- Cardiovasculaire risicofactoren: Hoe meer cardiovasculaire risicofactoren iemand had als kind en tiener - zoals obesitas, hoge bloeddruk en hoog cholesterolgehalte - hoe lager ze presteerden op geheugen- en denktesten na hun dertigste en 40e.
- Cardiorespiratoire fitheid verbeteren door sporten en bewegen kan ontstaan van prostaatkanker verminderen, blijkt uit Zweedse studie bij circa 50000 mannen
- Chemo en bestraling voor kinderen met kanker vergroot 6 tot 13 keer het risico op krijgen van borstkanker voor hun 40e jaar in vergelijking met bevolkingsrisico.
- Darmbarriere speelt een centrale rol in onze gezondheid. Verstoringen zorgen voor een groter risico op stofwisselingsziektes en speelt ook grote rol in immuniteit.
- Microbioom - Darmflora, een aantal artikelen bij elkaar gezet
- Darmkanker: Een periodieke colonoscopie - inwendig darmonderzoek - vermindert het risico op darmkanker stadium IIB of hoger met 70%.
- Depressie en angst leiden niet tot meer vormen van kanker blijkt uit jarenlang internationaal onderzoek
- Diabetes: Harmine, een natuurlijke alkaloide, blijkt de insuline productie te herstellen bij diabetes patienten en lijkt uitstekende behandeling om diabetes 1 en 2 te genezen
- Diagnostische fouten komen vaak voor in ziekenhuizen. 1 op de 14 patienten krijgt verkeerde diagnose maar is heel vaak te voorkomen.
- Gordelroosvaccin verlaagt risico met meer dan 20 procent op hart- en vaatziekten en blijft actief beschermen tot wel acht jaar na eerste vaccinatie
- Het Kytogeen dieet - koolhydraatarm dieet - strikt volgen kan schadelijk zijn. Lage hoeveelheid vezels en hoog vetgehalte leidt tot onevenwichtige darmflora.
- Hormoontherapie na de menopauze kan risico op kanker verhogen of verkleinen. Oestrogeen verhoogt. Oestrogeen plus Progesteen verkleint.
- HST - Hormoontherapie in en tijdens de overgang veroorzaakt 54 tot 93% kans op galwegziekte, aldus dubbelblinde gerandomiseerde studie bij ruim 14.000 gezonde vrouwen
- Infecties veroorzaken 16 procent van alle vormen van kanker wereldwijd. Leefstijl plus infecties zou voor 35 procent verantwoordelijk zijn aldus grote epidemologische studie in 184 landen
- Leefstijl en voeding in eerste twintig jaar van een mensenleven lijkt bepalend voor risico op krijgen van kanker toont grote Zweedse studie.
- Longkanker: Rauwe knoflook zou de kans op longkanker (44 procent) sterk verminderen. Blijkt uit groot Chinees onderzoek
- Mobiele telefoons geven verhoogd risico op kanker bij kinderen
- Nieuwe richtlijn ‘Overgewicht en obesitas bij volwassenen’ waarbij meetlint de weegschaal vervangt
- NIPT = Niet Invasieve Prenatale celvrije DNA-Test die geen resultaat laat zien of abnormale data betekent vaak (52 procent) dat de moeder beginnende kanker heeft blijkt uit de IDENTIFY studie
- Paddenstoelen: hogere dagelijkse consumptie van paddenstoelen geeft minder risico op krijgen van kanker. Verschil kan oplopen tot 47 procent.
- Parkinson: Aantal patienten met ziekte van Parkinson is schrikbarend gegroeit, vooral door milieuvervuiling als fijnstof en landbouwgif die worden gebruikt in de landbouw en tuinbouw
- PFAS producten lijken groter risico te geven op vormen van hormoongerelateerde kanker bij vrouwen, zoals eierstokkanker maar ook op een melanoom
- Ploegendienst met nachtdiensten vergroot de kans op het ontwikkelen van eierstokkanker
- Probiotica - melkzuurbacteriën kunnen in veel gevallen ziektes voorkomen of zorgen voor herstel van darmflora na chemo of bestraling
- Prostaatkanker: Dieet met groenten, fruit, vis, peulvruchten en volkoren granen vermindert duidelijk de kans op overlijden aan niet uitgezaaide prostaatkanker bij diagnose in vergelijking met westers dieet copy 1
- Psycho stimulerende middelen zoals Ritalin aan kinderen geeft verhoogde kans op krijgen van kanker later. Na 3 maanden ontstond een ernstige chromosoom afwijking. Fase III studie toegevoegd naar effecten van psycho stimulerende middelen op gezondheid
- ReCET - electroporation therapy is een nieuwe endoscopische behandeling en verbetert glykemische controle en stopt behoefte aan medisch toepassen van insuline bij patiënten met diabetes type 2
- Roken is nog schadelijker dan gedacht, maar stoppen met roken kan ook je leven verlengen.
- Screening: Draagbaar ultrasound scanapparaat blijkt uitstekende resultaten te geven bij ontdekken van kwaadaardige tumoren bij mensen met hoog risico op ontwikkelen van borstkanker
- Screeningtesten voor opsporen van kanker zoals voor borstkanker, longkanker, darmkanker en prostaatkanker lijken geen invloed te hebben op uiteindelijke levensduur
- Slaapmiddelen die regelmatig worden gebruikt door volwassenen zouden een 3 keer zo hoog risico geven eerder te sterven en meer kans op kanker in vergelijking met zelden of nooit slaapmiddelen gebruik
- Sociale stress zoals discriminatie en gezinsproblemen, samen met werk- en geldproblemen, kunnen bijdragen aan vroegtijdige veroudering van menselijk immuunsysteem
- Testosteronwaarde is sterk gerelateerd aan botdichtheidsverlies Bijna de helft van de mannen met een laag testosteron had osteopenie of osteoporose.
- Uromune vaccin is bijzonder effectief voor patiënten met recidiverende urineweginfecties (rUTI). 54 procent bleef 9 jaar gevrijwaard van een urineweginfectie zonder gebruik van antibiotica
- Vibratorgebruik kan de bekkengezondheid verbeteren bij vrouwen. Vibratorgebruik verbetert seksuele gezondheid, urine-incontinentie en vulvaire pijn
- Algemene informatie preventie



Plaats een reactie ...
Reageer op "PFAS producten lijken groter risico te geven op vormen van hormoongerelateerde kanker bij vrouwen, zoals eierstokkanker maar ook op een melanoom"