8 september 2017: Bron: The Lancet
Immuuntherapie met het vaccin rindopepimut faalt bij hersentumoren met een glioblastoom multiforme.
Dat ons projectvoorstel Utopie of Uitdaging zin heeft bewijst maar weer eens een grote fase III studie gepubliceerd in The Lancet. Immuuntherapie naast temodal - temozolomide met een vaccin (rindopepimut) gericht op de epidermal growth factor receptor (EGFR) mutatie EGFRvIII (30 % van glioblastoma patienten hebben die mutatie) bij nieuw gediagnosteerden van een hersentumor glioblastoma Multiforme waarbij na operatie weinig of geen zichtbaar rest tumorweefsel aantoonbaar is en de EGFR mutatie hadden, geeft geen enkel verschil in mediane overall overleving in vergelijking met alleen temodal - temozolomide.
 Beeld van een glioblastoom plus vocht eromheen
Beeld van een glioblastoom plus vocht eromheen
De studie werd uitgevoerd bij totaal 745 patiënten in 165 ziekenhuizen in 22 landen. Patiënten werden gerandomiseerd en blind ingedeeld in rindopepimut en temozolomide (n = 371) of controlegroep (placebo vaccin) en temozolomide (n = 374).
Studie werd uitgevoerd in periode van april 2012 tot december 2014 en gepubliceerd in The Lancet.
De overall overleving was exact geljik: 20.1 maanden in de rindopepimut groep vs 20.0 maanden in de controle groep (hazard ratio = 1.01, P = .93). Onder alle patienten in de "intent-to-treat" populatie, mediane overall overleving (OS) was 17.4 maanden vs 17.4 maanden in controlegroep (HR = 0.89, P = .22).
Ook was er weinig verschil in de bijwerkingen:
De meest voorkomende graad 3 of 4 bijwerkingen waren in de rindopepimut groep thrombocytopenia (9% vs 6% in controle groep), vermoeidheid (2% vs 5%), hersenvocht (2% vs 3%), wegvallen / epileptie aanvallen (2% vs 2%), en hoofdpijn (2% vs 3%). Ernstige bijwerkingen (>4) bleken epileptie aanvallen (5% vs 6%) en hersenvocht (2% vs 3%). 1 patient overleed aan de gevolgen van een longembolie die door de onderzoekers werd gezien als gerelateerd aan rindopepimut.
Onder de 745 patiënten, hadden 405 patiënten minimaal restweefsel, waarvan 195 patiënten waren ingedeeld in de rindopepimut groep en 210 in de controle groep. 338 patiënten hadden wel aantoonbaar resttumorweefsel.
Je vraagt je dan wel af waarom op basis van welke studiersultaten de FDA deze studie versneld goedkeurde
Hebben de onderzoekers gesjoemeld of heeft de FDA niet goed gekeken naar de eerdere studieresultaten? Het lijkt erop.
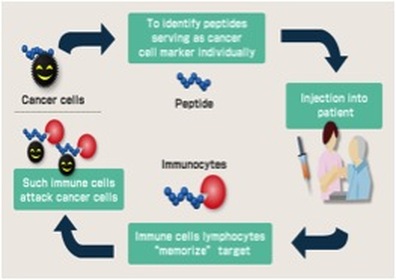
Rindopepimut (Rintega(R)) is an immunotherapy treatment under investigation, which works by targeting EGFRvIII, and reducing its ability to contribute to cancer growth. Rindopepimut is a peptide vaccine that binds to the corresponding 13-amino acid (molecules that make up proteins) “mutant vIII epitope,” which is connected to a carrier protein, KLH (for antibody production), which stimulates the immune system. Peptide vaccines are rapidly cycled and degraded in the body and therefore have minimal deleterious side effects. Peptides are naturally occurring biological molecules, which are made up of short chains of amino acids bonded together by peptide bonds (amine bonds). This peptide vaccine Rindopepimut, consists of using a peptide from the original pathogen, the cancer producing tumor in this case, to stimulate an immune response to fight the tumor. With the three Phase 2 trials of Rindopepimut (ACTIVATE, ACT II, and ACTIII) that have been carried out, the vaccine has been shown to inhibit the growth of EGFRvIII- expressing tumors in mouse models, suggesting that Rindopepimut has the capacity to improve both overall survival, and average survival without any progression of tumors. The vaccine seemingly initiates such a large immune response that 67% of patients who received Rindopepimut injectionss for 3 months or longer showed no visible expression of EGFRvIII. In addition, a Phase 3 study is underway, ACT IV, in newly diagnosed GBM, and a Phase 2 study, called ReACT for recurrent GBM patients. These studies are showing promising results, with noticeable increases in immune responses and health outcomes after just 3-4 months. These developments represent exciting steps in a process for immunotherapy to play a greater role in improving health outcomes, and especially for enabling immunotherapy treatment in brain cancer.
FDA Breakthrough Therapy Designation
As Rindopepimut has shown improvement in clinical outcomes over available therapy options, the FDA intends to speed up the development and review process of this drug through a “Breakthrough Therapy Designation.” The Breakthrough Therapy designation aims to accelerate the progress, analysis and review of Rindopepimut, which has the capacity to make huge advances in the treatment of such a severe and life threatening condition such as GBM.
Het volledige studierapport: Rindopepimut with temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double-blind, international phase 3 trial is tegen betlaing in te zien.
Hier het abstract van de studie:
In newly diagnosed EGFRvIII-positive glioblastoma, the addition of rindopepimut to temozolomide did not improve survival in patients with minimal residual disease.
Rindopepimut with temozolomide for patients with newly diagnosed, EGFRvIII-expressing glioblastoma (ACT IV): a randomised, double-blind, international phase 3 trial
Gerelateerde artikelen
- CAR-T celtherapie maakt dat kinderen met neuroblastoma nu in 2025 al meer dan 10 jaar kankervrij zijn. Met uitgelicht een prachtig overlevingsverhaal van een kind van 4 jaar die anno 2025 al 19 jaar kankervrij is. copy 1
- Immuuntherapie met specifieke CAR-T cel behandeling (GD2-CAR T cel behandeling) blijkt ook effectief bij kinderen en jong volwassen patienten met een hersentumor.
- CAR-T celtherapie rechtstreeks toegediend in de hersenen doet tumorweefsel van Glioblastoma Multiforma snel slinken en soms zelfs verdwijnen.
- Gepersonaliseerde vorm van immuuntherapie succesvol bij melanomen gegeven voor operatie doet hersentumor type Glioblastoma Multiforme van arts verdwijnen en er is nog geen teken van recidief na 1 jaar.
- mRNA vaccin doet hersentumoren type Glioblastoma razendsnel veranderen van koude tumoren in warme tumoren. Blijkt uit eerste klinische studie bij volwassen patienten en bevestigt resultaten uit dierstudies
- DCVax-L verbetert overall overleving en vermindert kans op recidief bij patiënten met nieuw gediagnosticeerd glioblastoom en recidiverend glioblastoom in vergelijking met beste standaardzorg
- Craniopharyngiomas, goedaardige inoperabele primaire hersentumoren van de hypofyse-hypothalamus-as met BRAF V600E mutaties reageren bijzonder goed op combinatiebehandeling van vemurafenib + cobimetinib
- Immuuntherapie met Natural Killer cellen en opgekweekte versterkte autologe T-cellen geeft verrassend goede resultaten bij patienten met een recidief van een hersentumor type glioblastoom multiforme
- Immuuntherapie met cocktail van 9 niet-toxische medicijnen - middelen bij hersentumoren van het type Glioblastoma Multiforme blijkt veilig en geeft veelbelovende resultaten bij eerste 9 patienten uit studie van prof. dr. Halatsch
- Lage tumor mutatie belasting geeft een langere overleving bij patienten met een recidief van een glioblastoom wanneer deze behandeld zijn met immuuntherapie met een gemoduleerd poliovirus of anti-PD medicijn
- Meisje van drie jaar komt en blijft in een complete remissie van een hersentumor glioblastoma met larotrectinib een zogeheten TRK medicijn op basis van haar ETV6–NTRK3 mutatie. copy 1
- Surviving terminal cancer: kunnen overlevenden van een hersentumor helpen kanker te overwinnen? Drie mannen overwonnen hun hersentumor - GBM - en 2 ervan zijn al 15 en 20 jaar vrij van kanker met eigen cocktail van bewezen niet-toxische middelen. copy 1 c
- Immuuntherapie met anti-PD medicijnen (pembrolizumab en / of nivolumab) geeft geen effect op overall overleving bij zwaar voorbehandelde patienten met glioblastoma multiforme
- Immuuntherapie met gemoduleerd poliovirus blijkt succesvol bij recidief van hersentumoren van het type glioblastoma multiforme graad IV
- Inovio Pharmaceuticals Initiates Immuno-Oncology Clinical Study for Glioblastoma in Combination with Regeneron’s PD-1 Inhibitor
- immuuntherapie met rindopepimut een vaccin (gericht op EGFR mutatie) naast temozolomide geeft geen enkel verschil in overall overleving in vergelijking met alleen temozolomide bij hersentumoren Glioblastoma met weinig of geen restweefsel na operatie
- Immuuntherapie met dendritische celtherapie voor hersentumoren type glioblastoma multiforme geeft 20 en 14 procent overall overleving versus 4 en 0 procent op 3 en 5 jaar .
- Dendritische celtherapie bij glioblastoma multiforme graad IV direct na bestraling plus temodal geeft langere overall overleving. 46 procent leeft nog na 3 jaar
- Nivolumab faalt bij recidief van een hersentumor Glioblastoma multiforme. Fase III studie Checkmate 143 wordt stopgezet
- Immuuntherapie met specifiek geprepareerde dendritische cellen (APVACS) plus tetanus virus (CMV) geeft superieure duurzame resultaten op ziektevrije tijd en overall overleving
- Immuuntherapie met gemoduleerd herpesvirus - AdV-Tk therapy - na operatie zorgt voor hoog significant meer en langere overleving in vergelijking met standaardbehandeling bij hersentumoren Glioblastoma multiforme
- APVACS - actief gepersonaliseerde vaccins - ontwikkelen tegen kanker wordt doel van nieuw consortium van 14 organisaties - GAPVAC, waaronder LUMC Leiden
- Toca 511 & Toca FC, een vorm van immuuntherapie met een gemodificeerd virus in combinatie met 5-FU bij hersentumoren - glioblastoma multiforme, heeft de eerste patiënt in behandeling genomen
- Dendritische celtherapie gecombineerd met een vaccin gericht op CD-133 eiwitexpressie voor patiënten met een hersentumor glioblastoma multiforme wordt in fase I/II studie onderzocht
- Behandeling met een virus - Delta-24-RDG - voor hersentumoren - glioblastoma multiforme wordt onderzocht in een fase I /II studie in het VUmc - Amsterdam
- Dendritische celtherapie gecombineerd met zogeheten mRNA's - cellen uit tumoren - verdriedubbeld overlevingstijd van mensen met een hersentumor - glioblastoma multiforme. copy 1
- Vaccin gemaakt van eigen tumorweefsel (HSPPC-96) verlengt leven 2 tot 3 keer zo lang van mensen met een geheel of gedeeltelijke operabele hersentumor. Dit.blijkt uit tussenevaluatie van fase II studie gepresenteerd op ASCO 2011
- Dendritische celtherapie met autoloog vaccin gebaseerd op antigenen geeft significant langere ziektevrije tijd en overall overleving bij patiënten met een hersentumor - glioblastoom
- Dendritische celtherapie vooral ook succesvol toepasbaar bij hersentumoren
- Immuuntherapie bij hersentumoren: Dendritische cellen toegediend na operatie van hersentumoren zorgt voor opmerkelijk goede kansen op geen recidief aldus resultaten uit kleinschalige studie bij 23 patiënten.
- Immuuntherapie bij hersentumoren: Dendritische cellen toegediend na operatie van hersentumoren zorgt voor opmerkelijk goede kansen op geen recidief aldus resultaten uit kleinschalige studie bij 12 patiënten.
- Immuuntherapie met synthetisch vaccin brengt enkele kinderen met een hersentumor - glioblastoom in een totale remissie
- Vaccin dat hersentumoren (Glioblastoom multiforme) met EGFRvIII expressie bestrijdt geeft verdubbeling van overlevingstijd en progressievrije tijd bij nieuw gediagnosteerde patienten
- Neuroblastomen: Immuuntherapie met chimeric anti-GD2 antibody ch 14.18 verhoogt significant overall overleving na 2 jaar met 20% t.o.v. alleen chemotherapie plus stamceltherapie.
- Stamcellen uit eigen bloed naast zware chemokuren geeft kinderen met recidief van hersentumoren langere overlevingstijd en kans op totale genezing, maar ook overlijdt 1 op de 4 kinderen aan de gevolgen van de behandeling
- Virussen: Herpes virusachtig medicijn - G207 wordt in fase I trial onderzocht bij kwaadaardige Glioma tumoren waarvoor radiotherapie - bestraling of chemo niet meer werkt en dus uitbehandeld zijn.
- Immuuntherapie bij hersentumoren met vaccins en virussen waaronder Newcastle Disease Virus. Een overzicht van recente ontwikkelingen.




 ACT IV trial investigators†
ACT IV trial investigators†
Plaats een reactie ...
Reageer op "immuuntherapie met rindopepimut een vaccin (gericht op EGFR mutatie) naast temozolomide geeft geen enkel verschil in overall overleving in vergelijking met alleen temozolomide bij hersentumoren Glioblastoma met weinig of geen restweefsel na operatie"