Mocht u kanker-actueel de moeite waard vinden en ons willen ondersteunen om kanker-actueel online te houden dan kunt u ons machtigen voor een periodieke donatie via donaties: https://kanker-actueel.nl/NL/donaties.html of doneer al of niet anoniem op - rekeningnummer NL79 RABO 0372931138 t.n.v. Stichting Gezondheid Actueel in Amersfoort. Onze IBANcode is NL79 RABO 0372 9311 38
Elk bedrag is welkom. En we zijn een ANBI instelling dus uw donatie of gift is in principe aftrekbaar voor de belasting.
22 november 2022: lees ook dit artikel: https://kanker-actueel.nl/NL/eerst-nier-verwijderen-en-daarna-behandelen-met-immuuntherapie-of-gerichte-therapie-geeft-betere-overall-overleving-bij-patienten-met-uitgezaaide-gevorderde-nierkanker-dan-zonder-nefrectomie.html
5 mei 2017: Bron: The Journal of Urology Jan. 2017 Volume 197
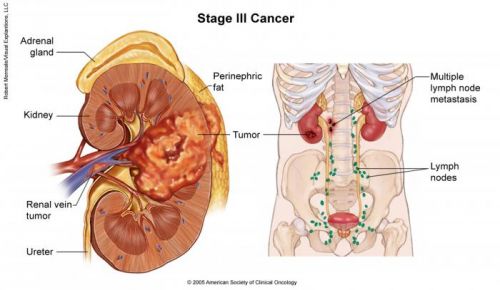
Wanneer bij patienten met uitgezaaide nierkanker (meestal uitgezaaid in omringende lymfklieren) de uitzaaiingen operatief worden verwijderd dan stijgen de kansen om te overleven met enkele jaren in vergelijking met als de uitzaaiingen niet worden verwijderd. Uit een meta analyse van 8 studies met totaal 2,267 patiënten met nierkanker kwam als resultaat dat de levensverwachting van gemiddeld 8 maanden tot 2 jaar bij de patiënten uit de groep die geen operatie kreeg, steeg naar 3 tot 12 jaar bij de patiënten waarbij de uitzaaiingen wel operatief waren verwijderd. En in die laatste groep bleken mensen ook echt genezen te zijn van uitgezaaide nierkanker.
Source: http://www.cancer.net/cancer-types/kidney-cancer/stages
Hoofdonderzoeker Bradley Leibovich, MD, een uroloog werkzaam in de Mayo Clinic zegt dat minder dan de helft van de patiënten, waarvan de uitzaaiingen werden verwijderd uiteindelijk toch kwamen te overlijden. Dit is een enorme verbetering, ook omdat met een operatie patienten dus bljkbaar genezen terwijl met medicijnen / chemokuren zelden een patiënt met uitgezaaide nierkanker ook echt geneest.
Leibovich: “Eerdere onderzoeken konden geen uitsluitsel geven over de effectiviteit van operatie, ondanks dat het bewijs ervoor wel aanwezig was. Door onze analyse van voorgaande onderzoeken zijn wij in staat gebleken het bewijs te leveren.”
Nierkanker kan op zich wel goed behandeld worden met medicijnen / chemotherapie. Maar dit onderzoek toont aan volgens dr. Leibovich dat de effectiviteit van behandelingen met medicijnen alleen geldt voor die patiënten die geen volledige verwijdering van de uitzaaiingen hebben gehad.
Bovendien verbetert de levensduur wel met medicijnen maar geneest het de patiënten niet.
Dr. Leibovich stelt: “Als medicijnen maar voor een beperkte tijd effectief werken terwijl operatie de overlevingskans aanzienlijk vergroot, dan zouden meer patiënten moeten overwegen om voor een operatie te kiezen.”
In een vervolgstudie wordt onderzocht of een combinatie van operatie en behandeling met medicijnen de kans op overleving en genezing nog meer kan verhogen.
Hier de 8 studies die in deze meta analyse zijn betrokken: (tekst gaat verder onder grafiek)
Characteristics of the 8 included studies
| References | Study Interval | Median Pt Age | Median Mos Followup | Histology (% clear cell) | Study Size | Median Mos OS | No. Organ Sites with Metastases (%) | % Systemic Therapy Received | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. CM | No. No CM | CM | No CM | CM | No CM | |||||||
| Alt et al14 | 1976–2006 | 63 | 33.6 | 90.20 | 125 | 762 | 48 | 15.6 | 1 (48), 2 or More (52) | Yes | Yes | |
| 45.60 | ||||||||||||
| Eggener et al15 | 1989–2007 | 61.7 | Not applicable | 80 | 40 | 89 | Pooled median OS 30 | Not applicable | Not applicable | Not applicable | ||
| Kavolius et al16 | 1980–1993 | 58 | Not applicable | Not applicable | 141 | 137 | 45 | 17 (no surgery), 20 (incomplete resection) | 1 (55.8), 2 or More (44.2) | Yes | Yes | |
| 12 | ||||||||||||
| Kwak et al17 | 1990–2004 | 60 | Not applicable | 85.70 | 21 | 41 | 36.5 | 8.4 | 1 (41.9), 2 or More (58.1) | Not applicable | Not applicable | |
| Meimarakis et al18 | 1986–2006 | 59.5 | Not applicable | 94.00 | 175 | 27 | 43.2 | 12.4 (R1 resection), 15.1 (R2 resection) | 1 (lung) (100) | Yes | Yes | |
| 28 | ||||||||||||
| Naito et al19 | 1988–2009 | 61 | 34.3 | 91.80 | 357 | 168 | Pooled median OS 80.1 | 1 (54.1), 2 or More (45.9) | Yes | Yes | ||
| 74.10 | ||||||||||||
| Staehler et al20 | 1995–2006 | 58 | 26 | 88 | 68 | 20 | 142 | 27 | 1 (liver) (100) | Yes | Yes | |
| 81 | ||||||||||||
| Yu et al21 | 2004–2013 | 57 | 45 | 93.80 | 31 | 65 | 52 | 22 (no surgery), 16 (incomplete resection) | 1 (63.5), 2 or More (36.5) | Yes | Yes | |
| 75 | ||||||||||||
Supplementary Appendix 2 (http://jurology.com/) summarizes the Cox multivariable models for each study, with 4 inclusive of some component of performance status (Karnofsky or ECOG).
Op de vraag of met de introductie van nieuwe medicijnen voor nierkanker de resultaten uit deze studie nu nog geldig zijn antwoordt dr. Leibovich het volgende en ik vertaal dit bewust niet om geen afbreuk te doen aan de uitspraak van dr. Leibovich:
Since the majority of the data analyzed in this study were published, immunotherapies and other drug therapies for kidney cancer have advanced considerably. The U.S. Food and Drug Administration approved the first drug for kidney cancer treatment in 1992, but there are more than 10 today, and most were approved in the past decade, according to the National Cancer Institute.
“Now that we have some better drugs for treating these patients, does our conclusion still hold true? We suspect that it will,” said Dr. Leibovich. “In people who haven't had complete removal of the metastases, drug therapy seems to benefit. But in patients who have that surgery, drug therapy doesn't seem to make a difference.”
Het volledige studierapport: Outcomes Following Complete Surgical Metastasectomy for Patients with Metastatic Renal Cell Carcinoma: A Systematic Review and Meta-Analysis is gratis n te zien.
Hier het abstract van deze studie:
Complete surgical metastasectomy for metastatic renal cell carcinoma is associated with improved survival compared with incomplete surgical metastasectomy based on meta-analysis of observational data. Consideration should be given to performing complete surgical metastasectomy, when technically feasible, in patients with metastatic renal cell carcinoma who are surgical candidates.
Outcomes Following Complete Surgical Metastasectomy for Patients with Metastatic Renal Cell Carcinoma: A Systematic Review and Meta-Analysis
Purpose
The benefit of complete surgical metastasectomy for patients with metastatic renal cell carcinoma remains controversial due to limited outcome data. We performed a systematic review and meta-analysis to determine whether complete surgical metastasectomy confers a survival benefit compared to incomplete or no metastasectomy for patients with metastatic renal cell carcinoma.
Materials and Methods
Ovid Embase®, MEDLINE®, Cochrane and Scopus® databases were searched for studies evaluating complete surgical metastasectomy for metastatic renal cell carcinoma through January 19, 2016. Only comparative studies reporting adjusted hazard ratios (aHRs) for all cause mortality of incomplete surgical metastasectomy vs complete surgical metastasectomy were included in the analysis. Generic inverse variance with random effects models was used to determine the pooled aHR. Risk of bias was assessed with the Newcastle-Ottawa Scale.
Results
Eight published cohort studies with a low or moderate potential for bias were included in the final analysis. The studies reported on a total of 2,267 patients (958 undergoing complete surgical metastasectomy and 1,309 incomplete surgical metastasectomy). Median overall survival ranged between 36.5 and 142 months for those undergoing complete surgical metastasectomy, compared to 8.4 to 27 months for incomplete surgical metastasectomy. Complete surgical metastasectomy was associated with a reduced risk of all cause mortality compared with incomplete surgical metastasectomy (pooled aHR 2.37, 95% CI 2.03–2.87, p <0.001), with low heterogeneity (I2 = 0%). Complete surgical metastasectomy remained independently associated with a reduction in mortality across a priori subgroup and sensitivity analyses, and regardless of whether we adjusted for performance status.
Conclusions
Complete surgical metastasectomy for metastatic renal cell carcinoma is associated with improved survival compared with incomplete surgical metastasectomy based on meta-analysis of observational data. Consideration should be given to performing complete surgical metastasectomy, when technically feasible, in patients with metastatic renal cell carcinoma who are surgical candidates.
References
No direct or indirect commercial incentive associated with publishing this article.
The corresponding author certifies that, when applicable, a statement(s) has been included in the manuscript documenting institutional review board, ethics committee or ethical review board study approval; principles of Helsinki Declaration were followed in lieu of formal ethics committee approval; institutional animal care and use committee approval; all human subjects provided written informed consent with guarantees of confidentiality; IRB approved protocol number; animal approved project number.
Supported by CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences, a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Gerelateerde artikelen
- Eerst nier verwijderen en daarna behandelen met immuuntherapie of gerichte therapie geeft betere overall overleving bij patienten met uitgezaaide gevorderde nierkanker dan zonder nefrectomie
- Regulier - nierkanker: actuele ontwikkelingen en belangrijke studies binnen de reguliere oncologie: een overzicht





Plaats een reactie ...
Reageer op "Operatieve verwijdering van uitzaaiingen vanuit nierkanker zorgt voor een jarenlange levensverlenging van 3 tot 12 jaar in vergelijking met geen operatie"