- 2.
Van Cutsem, E., Cervantes, A., Nordlinger, B., Arnold, D. & Group, E. G. W. Metastatic colorectal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 25(Suppl 3), iii1–iii9 (2014).
- 3.
National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Colon Cancer Version 2.2018. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed May 2018.
- 4.
Van Cutsem, E. et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann. Oncol. 27, 1386–1422 (2016).
- 5.
Douillard, J. Y. et al. Randomized, phase III trial of panitumumab with infusional fluorouracil, leucovorin, and oxaliplatin (FOLFOX4) versus FOLFOX4 alone as first-line treatment in patients with previously untreated metastatic colorectal cancer: the PRIME study. J. Clin. Oncol. 28, 4697–4705 (2010).
- 6.
Bokemeyer, C. et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann. Oncol. 22, 1535–1546 (2011).
- 7.
Clarke, C. N. & Kopetz, E. S. BRAF mutant colorectal cancer as a distinct subset of colorectal cancer: clinical characteristics, clinical behavior, and response to targeted therapies. J. Gastrointest. Oncol. 6, 660–667 (2015).
- 8.
Pietrantonio, F. et al. Predictive role of BRAF mutations in patients with advanced colorectal cancer receiving cetuximab and panitumumab: a meta-analysis. Eur. J. Cancer 51, 587–594 (2015).
- 9.
Rowland, A. et al. Meta-analysis of BRAF mutation as a predictive biomarker of benefit from anti-EGFR monoclonal antibody therapy for RAS wild-type metastatic colorectal cancer. Br. J. Cancer 112, 1888–1894 (2015).
- 10.
Jones, J. C. et al. Non-V600BRAF mutations define a clinically distinct molecular subtype of metastatic colorectal cancer. J. Clin. Oncol. 35, 2624–2630 (2017).
- 11.
Seligmann, J. F. et al. Association of tumor HER3 messenger RNA expression with panitumumab efficacy in advanced colorectal cancer. JAMA Oncol. 4, 564–568 (2018).
- 12.
Sartore-Bianchi, A., Marsoni, S. & Siena, S. Human epidermal growth factor receptor 2 as a molecular biomarker for metastatic colorectal cancer. JAMA Oncol. 4, 19–20 (2018).
- 13.
Scartozzi, M. et al. Analysis of HER-3, insulin growth factor-1, nuclear factor-kB and epidermal growth factor receptor gene copy number in the prediction of clinical outcome for K-RAS wild-type colorectal cancer patients receiving irinotecan-cetuximab. Ann. Oncol. 23, 1706–1712 (2012).
- 14.
Boeckx, N. et al. Primary tumor sidedness has an impact on prognosis and treatment outcome in metastatic colorectal cancer: results from two randomized first-line panitumumab studies. Ann. Oncol. 28, 1862–1868 (2017).
- 15.
Loupakis, F. et al. Primary tumor location as a prognostic factor in metastatic colorectal cancer. J. Natl. Cancer Inst. 107, dju427 (2015).
- 16.
Tejpar, S., Stintzing, S. & Ciardiello, F. Prognostic and predictive relevance of primary tumor location in patients with RAS wild-type metastatic colorectal cancer: Retrospective analyses of the CRYSTAL and FIRE-3 trials. JAMA Oncol. 3, 194–201 (2017).
- 17.
Petrelli, F., Tomasello, G. & Borgonovo, K. Prognostic survival associated with left-sided vs right-sided colon cancer: a systematic review and meta-analysis. JAMA Oncol. 3, 211–219 (2017).
- 18.
Stintzing, S., Tejpar, S., Gibbs, P., Thiebach, L. & Lenz, H. J. Understanding the role of primary tumour localisation in colorectal cancer treatment and outcomes. Eur. J. Cancer 84, 69–80 (2017).
- 19.
Boeckx, N. et al. The predictive value of primary tumor location in patients with metastatic colorectal cancer: a systematic review. Crit. Rev. Oncol. Hematol. 121, 1–10 (2018).
- 20.
Sartore-Bianchi, A. et al. Dual-targeted therapy with trastuzumab and lapatinib in treatment-refractory, KRAS codon 12/13 wild-type, HER2-positive metastatic colorectal cancer (HERACLES): a proof-of-concept, multicentre, open-label, phase 2 trial. Lancet Oncol. 17, 738–746 (2016).
- 21.
Guinney, J. et al. The consensus molecular subtypes of colorectal cancer. Nat. Med. 21, 1350–1356 (2015).
- 22.
Arnold, D. et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomised trials. Ann. Oncol. 28, 1713–1729 (2017).
- 23.
Holch, J. W., Ricard, I., Stintzing, S., Modest, D. P. & Heinemann, V. The relevance of primary tumour location in patients with metastatic colorectal cancer: A meta-analysis of first-line clinical trials. Eur. J. Cancer 70, 87–98 (2017).
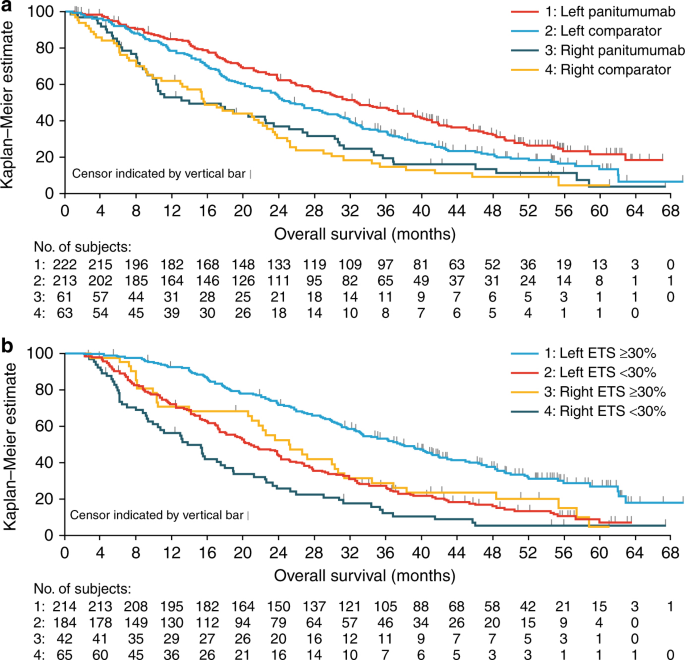
- 24.
Taieb, J. et al. Exploratory analyses assessing the impact of early tumour shrinkage and depth of response on survival outcomes in patients with RAS wild-type metastatic colorectal cancer receiving treatment in 3 randomised panitumumab trials. J. Cancer Res Clin. Oncol. 144, 321–335 (2018).
- 25.
Piessevaux, H. et al. Use of early tumor shrinkage to predict long-term outcome in metastatic colorectal cancer treated with cetuximab. J. Clin. Oncol. 31, 3764–3775 (2013).
- 26.
Douillard, J. Y. et al. Impact of early tumour shrinkage and resection on outcomes in patients with wild-type RAS metastatic colorectal cancer. Eur. J. Cancer 51, 1231–1242 (2015).
- 27.
Heinemann, V. et al. Early tumour shrinkage (ETS) and depth of response (DpR) in the treatment of patients with metastatic colorectal cancer (mCRC). Eur J Cancer 32, 1927–1936 (2015).
- 28.
Peeters M., et al. Impact of primary tumour location on response and resection outcomes in patients with metastatic colorectal cancer (mCRC) undergoing first-line treatment (abstract P-321). Ann Oncol. 28, 2017 https://doi.org/10.1093/annonc/mdx261.318
- 29.
Köhne C.-H., et al. Characteristics and response outcomes of long-term survivors in studies of first-line panitumumab for metastatic colorectal cancer (abstract P-319). Ann Oncol. 28, 2017 https://doi.org/10.1093/annonc/mdx261.316
- 30.
Douillard, J. Y. et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N. Engl. J. Med. 369, 1023–1034 (2013).
- 31.
Schwartzberg, L. S. et al. PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J. Clin. Oncol. 32, 2240–2247 (2014).
- 32.
Price, T. J. et al. Update on optimal treatment for metastatic colorectal cancer from the ACTG/AGITG expert meeting: ECCO 2015. Expert Rev. Anticancer Ther. 16, 557–571 (2016).
- 33.
Vogel, A., Hofheinz, R. D., Kubicka, S. & Arnold, D. Treatment decisions in metastatic colorectal cancer - beyond first and second line combination therapies. Cancer Treat. Rev. 59, 54–60 (2017).
- 34.
Kohne, C. H. et al. Clinical determinants of survival in patients with 5-fluorouracil-based treatment for metastatic colorectal cancer: results of a multivariate analysis of 3825 patients. Ann. Oncol. 13, 308–317 (2002).
- 35.
Folprecht, G. et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 11, 38–47 (2010).
- 36.
Geissler M., et al. mFOLFOXIRI + panitumumab versus FOLFOXIRI as first-line treatment in patients with RAS wild-type metastatic colorectal cancer m(CRC): a randomized phase II VOLFI trial of the AIO (AIO-KRK0109) (abstract 475O). Ann. Oncol. 28, 2017; https://doi.org/10.1093/annonc/mdx393.002
- 37.
Sobrero, A. et al. Impact of sequence of biologic therapies on overall survival (OS) in patients with RAS wild-type (WT) metastatic colorectal carcinoma (mCRC): an exploratory, retrospective pooled analysis (abstract P-149). Ann. Oncol. 27, ii44 (2016).
- 38.
Zaniboni, A. & Formica, V. The Best. First. Anti-EGFR before anti-VEGF, in the first-line treatment of RAS wild-type metastatic colorectal cancer: from bench to bedside. Cancer Chemother. Pharmacol. 78, 233–244 (2016).
- 39.
Folprecht, G. et al. Survival of patients with initially unresectable colorectal liver metastases treated with FOLFOX/cetuximab or FOLFIRI/cetuximab in a multidisciplinary concept (CELIM study). Ann. Oncol. 25, 1018–1025 (2014).
- 40.
Misale, S. et al. Emergence of KRAS mutations and acquired resistance to anti-EGFR therapy in colorectal cancer. Nature 486, 532–536 (2012).
- 41.
Siravegna, G. et al. Monitoring clonal evolution and resistance to EGFR blockade in the blood of metastatic colorectal cancer patients. Nat. Med. 21, 795–801 (2015).
- 42.
Santini, D. et al. Cetuximab rechallenge in metastatic colorectal cancer patients: how to come away from acquired resistance? Ann. Oncol. 23, 2313–2318 (2012).
- 43.
Ciardiello, F. et al. Cetuximab continuation after first progression in metastatic colorectal cancer (CAPRI-GOIM): a randomized phase II trial of FOLFOX plus cetuximab versus FOLFOX. Ann. Oncol. 27, 1055–1061 (2016).
- 44.
Siena S., et al. Rechallenge with EGFR inhibitors in patients with metastatic colorectal cancer: effect on outcomes (abstract P-320). Ann. Oncol. 28, 2017; https://doi.org/10.1093/annonc/mdx261.317
- 45.
Tonini, G., Imperatori, M., Vincenzi, B., Frezza, A. M. & Santini, D. Rechallenge therapy and treatment holiday: different strategies in management of metastatic colorectal cancer. J. Exp. Clin. Cancer Res. 32, 92 (2013).
Acknowledgements
We thank all patients, their families and all investigators involved in the PRIME and PEAK studies. Medical writing support (including development of a draft outline and subsequent drafts in consultation with the authors, assembling tables and figures, collating author comments, copyediting, fact checking and referencing) was provided by Louisa Lyon, DPhil and Louise Niven, DPhil at Aspire Scientific (Bollington, UK), and funded by Amgen (Europe) GmbH (Zug, Switzerland).
Author information
Affiliations
-
Department of Oncology, Antwerp University Hospital, Wilrijkstraat 10, 2650, Edegem, Belgium
- Marc Peeters
- & Timothy Price
-
Queen Elizabeth Hospital/University of Adelaide, 28 Woodville Rd, Woodville South, SA, 5011, Australia
- Timothy Price
-
Sorbonne Paris Cité, Paris Descartes University, Georges Pompidou European Hospital, 20 Rue Leblanc, 75015, Paris, France
- Julien Taieb
-
Klinikum Esslingen, Cancer Center Esslingen, Hirschlandstraße 97, 73730, Esslingen am Neckar, Germany
- Michael Geissler
-
Hospital Universitario Marqués de Valdecilla, Av. Valdecilla, 25, 39008, Santander, Spain
- Fernando Rivera
-
Service d’Oncologie-Hématologie, Grand Hôpital de Charleroi, Avenue du Centenaire 73, 6061, Charleroi, Belgium
- Jean-Luc Canon
-
Department of Medical Oncology, Ioannina University Hospital, Leof. Stavrou Niarchou, 455 00, Ioannina, Greece
- George Pentheroudakis
-
Biostatistics, Amgen Ltd, Sanderson Road, Uxbridge, UB8 1DH, UK
- Reija Koukakis
-
European Medical, Amgen (Europe) GmbH, Dammstrasse 23, 6300, Zug, Switzerland
- Peter Burdon
-
Dipartimento di Oncologia e Emato-Oncologia, Università degli Studi di Milano, Niguarda Cancer Center, Grande Ospedale Metropolitano Niguarda, Piazza dell’Ospedale Maggiore, 3, 20162, Milan, Italy
- Salvatore Siena
Contributions
R.K. and P.B. were responsible for conception and design of the analyses. T.P. and J.-L.C. contributed to the design of the analyses. M.P., T.P., J.T., F.R., J.-L.C. and S.S. contributed to patient data collection. RK performed the data analyses. All authors contributed to the interpretation of the data, the preparation and revision of the manuscript, and approved the final version.
Competing interests
M.P. has received research funding from Amgen, Roche and Sirtex, and honoraria from Amgen, Merck Serono, Roche, Sanofi Aventis, Servier and Sirtex. T.P. has acted on advisory boards for Amgen, Merck Serono and Roche, and has received travel support from Amgen. J.T. has acted in consultancy and/or advisory roles for, and received honoraria from Amgen, Baxalta, Celgene, Eli Lilly, Merck, Roche, Sanofi, Servier and Sirtex. Michael Geissler has received research funding and acted in consultancy/advisory roles for Amgen, Bayer, Merck, Roche and Sanofi. F.R. has received research funding from and/or acted on advisory boards for Amgen, Bayer, Celgene, Eli Lilly, Merck Serono, Merck Sharp & Dohme, Roche, Servier and Sanofi. J.-L.C. is a consultant/advisor for Amgen and Roche and has received institutional funding from Amgen, Novartis and Roche. G.P. has received research funding and advisory consulting fees from Amgen, Astra Zeneca, Boehringer, Bristol Myers Squibb, Lilly, Merck, MSD and Roche. R.K. is an employee of Amgen Ltd and owns restricted shares in Amgen. P.B. is an employee of Amgen (Europe) GmbH and owns shares in Amgen. S.S. is a member of advisory boards for Amgen, Bayer, Celgene, Eli Lilly, Ignyta, Merck, Merrimack, Novartis, Roche and Sanofi.
Consent to participate
All patients provided informed consent.
Ethics approval
The PRIME and PEAK studies were conducted in accordance with the Declaration of Helsinki. Study protocols were approved by an independent ethics committee at each study center.
Funding
The PRIME (NCT00364013) and PEAK (NCT00819780) studies were supported by Amgen Inc.
Corresponding author
Correspondence to Marc Peeters.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.



Plaats een reactie ...
Reageer op "Plaats van de primaire tumor bij uitgezaaide darmkanker geeft grote verschillen in overall overleving bij patiënten met RAS wild-type die eerstelijns behandeling met panitumumab krijgen"