Abstract
Gastric and gastroesophageal junction (G/GEJ) cancers carry a poor prognosis, and despite recent advancements, most patients die of their disease. Although immune checkpoint blockade became part of the standard-of-care for patients with metastatic G/GEJ cancers, its efficacy and impact on the tumor microenvironment (TME) in early disease remain largely unknown. We hypothesized higher efficacy of neoadjuvant immunotherapy plus chemotherapy in patients with nonmetastatic G/GEJ cancer. In the phase 2 PANDA trial, patients with previously untreated resectable G/GEJ tumors (n = 21) received neoadjuvant treatment with one cycle of atezolizumab monotherapy followed by four cycles of atezolizumab plus docetaxel, oxaliplatin and capecitabine. Treatment was well tolerated. There were grade 3 immune-related adverse events in two of 20 patients (10%) but no grade 4 or 5 immune-related adverse events, and all patients underwent resection without treatment-related delays, meeting the primary endpoint of safety and feasibility. Tissue was obtained at multiple time points, allowing analysis of the effects of single-agent anti-programmed cell death ligand 1 (PD-L1) and the subsequent combination with chemotherapy on the TME. Twenty of 21 patients underwent surgery and were evaluable for secondary pathologic response and survival endpoints, and 19 were evaluable for exploratory translational analyses. A major pathologic response (≤10% residual viable tumor) was observed in 14 of 20 (70%, 95% confidence interval 46–88%) patients, including 9 (45%, 95% confidence interval 23–68%) pathologic complete responses. At a median follow-up of 47 months, 13 of 14 responders were alive and disease-free, and five of six nonresponders had died as a result of recurrence. Notably, baseline anti-programmed cell death protein 1 (PD-1)+CD8+ T cell infiltration was significantly higher in responders versus nonresponders, and comparison of TME alterations following anti-PD-L1 monotherapy versus the subsequent combination with chemotherapy showed an increased immune activation on single-agent PD-1/L1 axis blockade. On the basis of these data, monotherapy anti-PD-L1 before its combination with chemotherapy warrants further exploration and validation in a larger cohort of patients with nonmetastatic G/GEJ cancer. ClinicalTrials.gov registration: NCT03448835.
Similar content being viewed by others

Neoadjuvant therapy with immune checkpoint blockade, antiangiogenesis, and chemotherapy for locally advanced gastric cancer

Current developments in gastric cancer: from molecular profiling to treatment strategy
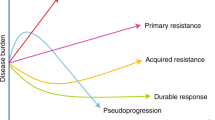
Resistance to immune checkpoint inhibitors in advanced gastro-oesophageal cancers
Data availability
The RNA and DNA sequencing data will be deposited in the European Genome-Phenome Archive under EGAS00001007676, and these data will be shared on reasonable request for academic use and within the limitations of the provided informed consent and under General Data Protection Regulation law. All data requests supported by the principal investigator/corresponding author of the study will be reviewed by the institutional review board of the NKI. The researcher will need to sign a data access agreement with the NKI after approval. The form to request access can be found at https://ega.nki.nl/ and will be centrally reviewed through repository@nki.nl, which will contact the corresponding author (M.C.). Estimated time to response is 2–4 weeks.
References
-
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
-
Shapiro, J. et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 16, 1090–1098 (2015).
-
Al-Batran, S. E. et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. Lancet 393, 1948–1957 (2019).
-
Al-Batran, S. E. et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 17, 1697–1708 (2016).
-
Thompson, E.D. et al. Patterns of PD-L1 expression and CD8 T cell infiltration in gastric adenocarcinomas and associated immune stroma. Gut 66, 794–801 (2017).
-
Kawazoe, A. et al. Clinicopathological features of programmed death ligand 1 expression with tumor-infiltrating lymphocyte, mismatch repair, and Epstein–Barr virus status in a large cohort of gastric cancer patients. Gastric Cancer 20, 407–415 (2017).
-
Geng, Y. et al. Expression of costimulatory molecules B7-H1, B7-H4 and Foxp3+ Tregs in gastric cancer and its clinical significance. Int. J. Clin. Oncol. 20, 273–281 (2015).
-
Gu, L. et al. PD-L1 and gastric cancer prognosis: a systematic review and meta-analysis. PLoS ONE12, e0182692 (2017).
-
Bang, Y.-J. et al. Pembrolizumab alone or in combination with chemotherapy as first-line therapy for patients with advanced gastric or gastroesophageal junction adenocarcinoma: results from the phase II nonrandomized KEYNOTE-059 study. Gastric Cancer 22, 828–837 (2019).
-
Janjigian, Y. Y. et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet 398, 27–40 (2021).
-
Kelly, R. J. et al. Adjuvant nivolumab in resected esophageal or gastroesophageal junction cancer. N. Engl. J. Med. 384, 1191–1203 (2021).
-
Amaria, R. N. et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat. Med. 24, 1649–1654 (2018).
-
Blank, C. U. et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat. Med. 24, 1655–1661 (2018).
-
Huang, A. C. et al. A single dose of neoadjuvant PD-1 blockade predicts clinical outcomes in resectable melanoma. Nat. Med. 25, 454–461 (2019).
-
Forde, P. M. et al. Neoadjuvant PD-1 blockade in resectable lung cancer. N. Engl. J. Med. 378, 1976–1986 (2018).
-
Powles, T. et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat. Med. 25, 1706–1714 (2019).
-
Chalabi, M. et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat. Med. 26, 566–576 (2020).
-
Cercek, A. et al. PD-1 blockade in mismatch repair-deficient, locally advanced rectal cancer. N. Engl. J. Med. 386, 2363–2376 (2022).
-
Versluis, J. M., Long, G. V. & Blank, C. U. Learning from clinical trials of neoadjuvant checkpoint blockade. Nat. Med. 26, 475–484 (2020).
-
Reijers, I. L. M. et al. The interferon-gamma (IFN-y) signature from baseline tumor material predicts pathologic response after neoadjuvant ipilimumab (IPI) + nivolumab (NIVO) in stage III melanoma. J. Clin. Oncol. 40, 9539–9539 (2022).
-
Bailly, C., Thuru, X. & Quesnel, B. Combined cytotoxic chemotherapy and immunotherapy of cancer: modern times. NAR Cancer 2, zcaa002 (2020).
-
Xue, Y. et al. Platinum-based chemotherapy in combination with PD-1/PD-L1 inhibitors: preclinical and clinical studies and mechanism of action. Expert Opin. Drug Deliv. 18, 187–203 (2021).
-
Golchin, S., Alimohammadi, R., Rostami Nejad, M. & Jalali, S. A. Synergistic antitumor effect of anti-PD-L1 combined with oxaliplatin on a mouse tumor model. J. Cell Physiol. 234, 19866–19874 (2019).
-
Loibl, S. et al. A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: clinical results and biomarker analysis of GeparNuevo study. Ann. Oncol. 30, 1279–1288 (2019).
-
Loibl, S. et al. Neoadjuvant durvalumab improves survival in early triple-negative breast cancer independent of pathological complete response. Ann. Oncol. 33, 1149–1158 (2022).
-
Tetzlaff, M. T. et al. Pathological assessment of resection specimens after neoadjuvant therapy for metastatic melanoma. Ann. Oncol. 29, 1861–1868 (2018).
-
Cottrell, T. R. et al. Pathologic features of response to neoadjuvant anti-PD-1 in resected non-small-cell lung carcinoma: a proposal for quantitative immune-related pathologic response criteria (irPRC). Ann. Oncol. 29, 1853–1860 (2018).
-
Vos, J. L. et al. FDG-PET accurately identifies pathological response early upon neoadjuvant immune checkpoint blockade in head and neck squamous cell carcinoma. Eur. J. Nucl. Med. Mol. Imaging 49, 2010–2022 (2022).
-
Reijers, I. L. M. et al. Personalized response-directed surgery and adjuvant therapy after neoadjuvant ipilimumab and nivolumab in high-risk stage III melanoma: the PRADO trial. Nat. Med. 28, 1178–1188 (2022).
-
Rozeman, E. A. et al. Survival and biomarker analyses from the OpACIN-neo and OpACIN neoadjuvant immunotherapy trials in stage III melanoma. Nat. Med. 27, 256–263 (2021).
-
Cascone, T. et al. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial. Nat. Med. 27, 504–514 (2021).
-
Gros, A. et al. PD-1 identifies the patient-specific CD8+ tumor-reactive repertoire infiltrating human tumors. J. Clin. Invest. 124, 2246–2259 (2014).
-
Hummelink, K. et al. PD-1T TILs as a predictive biomarker for clinical benefit to PD-1 blockade in patients with advanced NSCLC. Clin. Cancer Res. 28, 4893–4906 (2022).
-
Thommen, D. S. et al. A transcriptionally and functionally distinct PD-1(+) CD8(+) T cell pool with predictive potential in non-small-cell lung cancer treated with PD-1 blockade. Nat. Med. 24, 994–1004 (2018).
-
Duhen, T. et al. Co-expression of CD39 and CD103 identifies tumor-reactive CD8 T cells in human solid tumors. Nat. Commun. 9, 2724 (2018).
-
Ayers, M. et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Invest. 127, 2930–2940 (2017).
-
Schumacher, T. N. & Thommen, D. S. Tertiary lymphoid structures in cancer. Science 375, eabf9419 (2022).
-
Siddiqui, I. et al. Intratumoral Tcf1(+)PD-1(+)CD8(+) T cells with stem-like properties promote tumor control in response to vaccination and checkpoint blockade immunotherapy. Immunity 50, 195–211.e110 (2019).
-
Zhao, X., Shan, Q. & Xue, H. H. TCF1 in T cell immunity: a broadened frontier. Nat. Rev. Immunol. 22, 147–157 (2022).
-
Krystel-Whittemore, M., Dileepan, K. N. & Wood, J. G. Mast cell: a multi-functional master cell. Front Immunol. 6, 620 (2015).
-
Network, C.G.A.R. Comprehensive molecular characterization of gastric adenocarcinoma. Nature 513, 202–209 (2014).
-
Chen, Y. et al. Predicting response to immunotherapy in gastric cancer via multi-dimensional analyses of the tumour immune microenvironment. Nat. Commun. 13, 4851 (2022).
-
Basham, T. Y. & Merigan, T. C. Recombinant interferon-gamma increases HLA-DR synthesis and expression. J. Immunol. 130, 1492–1494 (1983).
-
Blomberg, O. S. et al. IL-5-producing CD4(+) T cells and eosinophils cooperate to enhance response to immune checkpoint blockade in breast cancer. Cancer Cell 41, 106–123.e110 (2023).
-
Cunningham, D. et al. Peri-operative chemotherapy with or without bevacizumab in operable oesophagogastric adenocarcinoma (UK Medical Research Council ST03): primary analysis results of a multicentre, open-label, randomised phase 2–3 trial. Lancet Oncol. 18, 357–370 (2017).
-
Lombardi, P. M. et al. Prognostic value of pathological tumor regression grade in locally advanced gastric cancer: new perspectives from a single‐center experience. J. Surg. Oncol. 123, 923–931 (2021).
-
Huffman, B. M. et al. Analysis of circulating tumor DNA to predict risk of recurrence in patients with esophageal and gastric cancers. JCO Precis. Oncol. 6, e2200420 (2022).
-
Kotani, D. et al. Molecular residual disease and efficacy of adjuvant chemotherapy in patients with colorectal cancer. Nat. Med. 29, 127–134 (2023).
-
Janjigian, Y. et al. LBA73 Pathological complete response (pCR) to durvalumab plus 5-fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT) in resectable gastric and gastroesophageal junction cancer (GC/GEJC): interim results of the global, phase III MATTERHORN study. Ann. Oncol. 34, S1315–S1316 (2023).
-
Gordon, A. et al. Primary results of the ICONIC phase 2 trial of perioperative FLOT plus avelumab (FLOT-A) in operable oesophagogastric adenocarcinoma (OGA). J. Clin. Oncol. 41, 446–446 (2023).
-
van Hagen, P. et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N. Engl. J. Med. 366, 2074–2084 (2012).
-
Lorenzen, S. et al. Perioperative atezolizumab plus fluorouracil, leucovorin, oxaliplatin, and docetaxel for resectable esophagogastric cancer: interim results from the Randomized, Multicenter, Phase II/III DANTE/IKF-s633 Trial. J. Clin. Oncol. https://doi.org/10.1200/JCO.23.00975 (2023).
-
Guo, H. et al. Efficacy and safety of sintilimab plus XELOX as a neoadjuvant regimen in patients with locally advanced gastric cancer: a single-arm, open-label, phase II trial. Front. Oncol. 12, 927781 (2022).
-
Yin, Y. et al. Neoadjuvant tislelizumab and tegafur/gimeracil/octeracil (S-1) plus oxaliplatin in patients with locally advanced gastric or gastroesophageal junction cancer: early results of a phase 2, single-arm trial. Front. Oncol. 12, 959295 (2022).
-
Jiang, H. et al. Efficacy and safety of neoadjuvant sintilimab, oxaliplatin and capecitabine in patients with locally advanced, resectable gastric or gastroesophageal junction adenocarcinoma: early results of a phase 2 study. J. Immunother. Cancer 10, e003635 (2022).
-
Tang, X. et al. Neoadjuvant PD-1 blockade plus chemotherapy induces a high pathological complete response rate and anti-tumor immune subsets in clinical stage III gastric cancer. Oncoimmunology 11, 2135819 (2022).
-
Shitara, K., et al. Neoadjuvant and adjuvant pembrolizumab plus chemotherapy in locally advanced gastric or gastrooesophageal cancer (KEYNOTE-585): an interim analysis of the multicentre, double-blind, randomised phase 3 study. Lancet Oncol. https://doi.org/10.1016/S1470-2045(23)00541-7 (2023).
-
Klempner, S. et al. Sequential pembrolizumab cooperates with platinum/5FU to remodel the tumor immune microenvironment in advanced gastric cancer: a phase II chemoimmunotherapy trial. Preprint at Research Square https://doi.org/10.21203/rs.3.rs-2793348/v1 (2023).
-
Li, S. et al. Neoadjuvant therapy with immune checkpoint blockade, antiangiogenesis, and chemotherapy for locally advanced gastric cancer. Nat. Commun. 14, 8 (2023).
-
Al-Batran, S.-E. et al. Surgical and pathological outcome, and pathological regression, in patients receiving perioperative atezolizumab in combination with FLOT chemotherapy versus FLOT alone for resectable esophagogastric adenocarcinoma: interim results from DANTE, a randomized, multicenter, phase IIb trial of the FLOT-AIO German Gastric Cancer Group and Swiss SAKK. J. Clin. Oncol. 40, 4003–4003 (2022).
-
van der Werf, L. R., Busweiler, L. A. D., van Sandick, J. W., van Berge Henegouwen, M. I. & Wijnhoven, B. P. L. Reporting national outcomes after esophagectomy and gastrectomy according to the esophageal complications consensus Group (ECCG). Ann. Surg. 271, 1095–1101 (2020).
-
Voeten, D. M. et al. Outcomes of esophagogastric cancer surgery during eight years of surgical auditing by the dutch upper gastrointestinal cancer audit (DUCA). Ann. Surg. 274, 866–873 (2021).
-
Blomberg, O. S. et al. Neoadjuvant immune checkpoint blockade triggers persistent and systemic T(reg) activation which blunts therapeutic efficacy against metastatic spread of breast tumors. Oncoimmunology 12, 2201147 (2023).
-
Arce Vargas, F. et al. Fc effector function contributes to the activity of human anti-CTLA-4 antibodies. Cancer Cell 33, 649–663.e644 (2018).
-
Waight, J. D. et al. Selective FcγR co-engagement on APCs modulates the activity of therapeutic antibodies targeting T cell antigens. Cancer Cell 33, 1033–1047.e1035 (2018).
-
Haruna, M. et al. The impact of CCR8+ regulatory T cells on cytotoxic T cell function in human lung cancer. Sci. Rep. 12, 5377 (2022).
-
Kidani, Y. et al. CCR8-targeted specific depletion of clonally expanded Treg cells in tumor tissues evokes potent tumor immunity with long-lasting memory. Proc. Natl Acad. Sci. USA 119, e2114282119 (2022).
-
Amin, M. B. et al. The eighth edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more ‘personalized’ approach to cancer staging. CA Cancer J. Clin. 67, 93–99 (2017).
-
Revised common terminology criteria for adverse events (CTCAE) version 4.0. National Cancer Institute https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm#ctc_40 (2009).
-
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2009).
-
Bartley, A. N. et al. HER2 testing and clinical decision making in gastroesophageal adenocarcinoma: guideline from the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. J. Clin. Oncol. 35, 446–464 (2017).
-
Mandard, A. M. et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 73, 2680–2686 (1994).
-
Travis, W. D. et al. IASLC Multidisciplinary recommendations for pathologic assessment of lung cancer resection specimens after neoadjuvant therapy. J. Thorac. Oncol. 15, 709–740 (2020).
-
Stringer, C., Wang, T., Michaelos, M. & Pachitariu, M. Cellpose: a generalist algorithm for cellular segmentation. Nat. Methods 18, 100–106 (2021).
-
Bankhead, P. et al. QuPath: open source software for digital pathology image analysis. Sci. Rep. 7, 16878 (2017).
-
Ijsselsteijn, M. E., van der Breggen, R., Farina Sarasqueta, A., Koning, F. & de Miranda, N. A 40-marker panel for high dimensional characterization of cancer immune microenvironments by imaging mass cytometry. Front. Immunol. 10, 2534 (2019).
-
Somarakis, A., Van Unen, V., Koning, F., Lelieveldt, B. & Hollt, T. ImaCytE: visual exploration of cellular micro-environments for imaging mass cytometry data. IEEE Trans. Vis. Comput. Graph. 27, 98–110 (2021).
-
Höllt, T. et al. Cytosplore: interactive immune cell phenotyping for large single‐cell datasets. Comput. Graph. Forum 35, 171–180 (2016).
-
Priestley, P. et al. Pan-cancer whole-genome analyses of metastatic solid tumours. Nature 575, 210–216 (2019).
-
Alexandrov, L. B. et al. The repertoire of mutational signatures in human cancer. Nature 578, 94–101 (2020).
-
Danaher, P. et al. Gene expression markers of tumor infiltrating leukocytes. J. Immunother. Cancer 5, 18 (2017).
-
de Vries, N. L. et al. γδ T cells are effectors of immunotherapy in cancers with HLA class I defects. Nature 613, 743–750 (2023).
-
Reinert, T. et al. Analysis of plasma cell-free DNA by ultradeep sequencing in patients with stages I to III colorectal cancer. JAMA Oncol. 5, 1124–1131 (2019).
Acknowledgements
We thank Hoffman-La Roche for funding this study. We thank all the patients and their families for participating in the present study. We thank the Core Facility of Molecular Pathology and Biobanking, in particular A. Broeks, S. Cornelissen and M. Alkemade, for their support in processing samples and performing immunohistochemistry; M. Nieuwland, R. Kluin, A. Velds and the Genomics Core Facility for their support with sequencing; I. Seignette for her support in digital imaging analysis using HALO; R. Harkes and Y. Ge for their support in quantification of CD8+ cells using QuPath; L. Al-van Wijck and M. van de Belt from the scientific administration department for data management and for support in trial conduct and management; N. Brandhorst for facilitating sample acquisition and processing; T. Korse, M. Lucas and E. Platte for PBMC acquisition and processing; Y. Hilhorst and M. Warmerdam for patient care; and St Jansdal Hospital, Rode Kruis Hospital, Tergooi Medical Center, Haga Hospital, Noordwest Hospital Group, Gelre Hospitals, Amsterdam UMC, Franciscus Hospital, PoliDirect IJburg, Slotervaart Hospital, Laurentius Hospital and St Antonius Hospital for patient referral. We would also like to acknowledge M.C. Liu and G. Laliotis from Natera for their supervision and critical review of the ctDNA analysis. The present study was funded by Hoffman-La Roche and sponsored by the NKI. The funding source had no role in design and execution of the study, data analysis or writing of the manuscript.
Author information
-
These authors contributed equally: Joris van de Haar, José G. van den Berg.
Authors and Affiliations
-
Department of Gastrointestinal Oncology, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Yara L. Verschoor, Jolanda M. van Dieren, Cecile Grootscholten, Marieke A. Vollebergh, Peggy den Hartog, Monique E. van Leerdam, Emile E. Voest & Myriam Chalabi
-
Department of Molecular Oncology and Immunology, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Joris van de Haar, Ton N. Schumacher & Emile E. Voest
-
Oncode Institute, Amsterdam, the Netherlands
Joris van de Haar, Ton N. Schumacher & Emile E. Voest
-
Department of Pathology, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
José G. van den Berg & Liudmila L. Kodach
-
Department of Surgery, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Johanna W. van Sandick, Alexander A. F. A. Veenhof & Koen J. Hartemink
-
Biometrics department, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Sara Balduzzi
-
Department of Pathology, Leiden University Medical Center, Leiden, the Netherlands
Marieke E. IJsselsteijn & Noel F. C. C. de Miranda
-
Department of Medical Oncology, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Marieke A. Vollebergh, John B. A. G. Haanen & Myriam Chalabi
-
Natera, Inc, Austin, TX, USA
Adham Jurdi, Shruti Sharma & Erik Spickard
-
Department of Nuclear Medicine, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Emilia C. Owers
-
Department of Radiology, Netherlands Cancer Institute – Antoni van Leeuwenhoek Hospital, Amsterdam, the Netherlands
Annemarieke Bartels-Rutten
-
Department of Gastroenterology and Hepatology, Leiden University Medical Center, Leiden, the Netherlands
Monique E. van Leerdam
-
Department of Medical Oncology, Leiden University Medical Center, Leiden, the Netherlands
John B. A. G. Haanen
-
Oncology Service, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland
John B. A. G. Haanen
-
Department of Hematology, Leiden University Medical Center, Leiden, the Netherlands
Ton N. Schumacher
Contributions
Y.L.V. analyzed and interpreted clinical and translational data and wrote the manuscript under supervision of M.C. J.v.d.H performed the genomic/transcriptomic biomarker analyses. S.B. performed statistical analyses. J.G.v.d.B. and L.L.K. performed the histo- and immunopathologic scoring. J.G.v.d.B. annotated tumor areas for IHC quantification analysis. M.E.I. and N.F.C.C.d.M. performed IMC and interpreted the data. A.J., S.S., E.S. performed ctDNA analysis and interpreted the data together with Y.L.V. and M.C. C.G., M.A.V. and P.d.H. were responsible for patient care. J.W.v.S., A.A.F.A.V. and K.J.H. informed patients and performed surgery. J.M.v.D. and M.E.v.L. performed endoscopies. J.M.v.D. revised all endoscopic reports and images. A.B.-R. revised CT scans, and E.C.O. revised FDG-PET scans. M.C., T.N.S. and J.B.A.G.H. made the experimental plan of investigation. M.C. designed the trial and coordinated trial procedures. All authors reviewed, edited and approved the manuscript and vouch for the accuracy of the data reported and adherence to the protocol.
Corresponding author
Correspondence to Myriam Chalabi.



Plaats een reactie ...
Reageer op "Immuuntherapie vooraf aan operatie en chemotherapie blijkt succesvol bij kankerpatiënten met maagkanker en met tumoren op de overgang van slokdarm naar de maag"