3 april 2021: lees ook dit artikel: https://kanker-actueel.nl/kytogeen-dieet-bij-patienten-met-eierstokkanker-en-endometriosekanker-verbetert-fysiek-functioneren-vergroot-de-energie-vermindert-vermoeidheid-en-vermindert-hongergevoel.html
19 maart 2018: lees ook deze artikelen:
en dit artikel:
En dit artikel:
en dit artikel:
19 maart 2018: Bron: Brouns, F. Eur J Nutr (2018). https://doi.org/10.1007/s00394-018-1636-y
Dat een zo laag mogelijke inname van suiker het risico op overgewicht en diabetes vermindert, is al vaker bewezen in internationale studies. Maar uit Nederlands en internationaal onderzoek blijkt ook dat het strikt volgen van een koolhydraatarm dieet (ketygeen-dieet) vooral door de lage hoeveelheid vezels en het hoge vetgehalte van een koolhydraatarm dieet kan leiden tot een onevenwichtige darmflora, aldus dr. Brouns, emeritus hoogleraar Innovatie in Gezonde Voeding verbonden aan de Universiteit van Maastricht op basis van internationaal onderzoek waar hij aan heeft meegewerkt. (Tekst gaat verder onder grafiek)
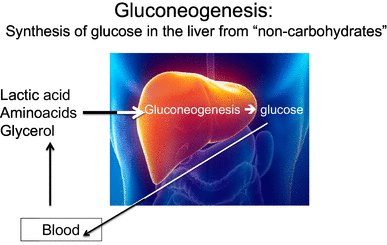
Gluconeogenesis (production of glucose) and glycolysis (breakdown of glucose) are processes that always take place simultaneously and are reciprocal (if one is high, the other is low, and vice versa). In cases of low-glucose availability from glycogen, glycolysis will be conducted at a low level and there will be a stimulus for gluconeogenesis
Een ketogeen dieet blijkt voor velen ook moeilijk vol te houden. In plaats daarvan zou een matig veranderd voedingspatroon dat minimaal 100 tot 150 gram koolhydraten per dag levert beter vol te houden zijn, zegt dr. Brouns in het Algemeen Dagblad als toelichting op zijn onderzoek.
In Wikipedia staat dit schema van koolhydraatarme dieëten:
| Typen ketogene diëten[1] | ||||
|---|---|---|---|---|
| Typen ketogene diëten | Vet (% totale energie-inname) | Eiwit (% totale energie-inname) | Koolhydraten (% totale energie-inname) | Opmerkingen |
| Klassiek ketogeen dieet | LCT: 85–90 | 6-8 | 2-4 | Verhouding tussen vet en niet-vet tussen 3:1 en 4:1. Slechte compliance. Constipatie treedt vaak op |
| MCT dieet | MCT: 71 | 10 | 19 | Verhouding tussen vet en niet-vet is 3:1. Gemakkelijker te bereiden. Misselijkheid, overgeven en diarree bij circa 50% van de patiënten |
| Gemodificeerd MCT dieet | LCT: 40–50 & MCT: 30 | 10-20 | 5-10 | Zowel LCT's als MCT's. Minder bijverschijnselen |
| Gemodificeerd Atkins dieet | 60–70 | 20-30 | 5 | Geen vasten of ziekenhuisopname. Geen restrictie op calorie-inname |
| Laag-glycemische-index dieet | 60–70 | 20-30 | 10 | Uitsluitend laag-GI koolhydraten toegestaan voor de 10% dagelijkse koolhydraten. |
| Bronnen, noten en/of referenties |
(en) Misiewicz Runyon A, So T-Y The use of ketogenic diet in pediatric patients with epilepsy. ISRN Pediatr. 2012:263139. DOI:10.5402/2012/263139. PMID 22970384. Dit is een open access artikel, beschikbaar onder de licentie Creative Commons Naamsvermelding (CC BY).
Dr. Brouns verwijst daarbij naar een recent internationaal onderzoek naar voedselrichtlijnen waaraan hij meewerkte. In deze studie werden richtlijnen van 11 landen en instanties zoals de Wereldgezondheidsorganisatie en de Europese Autoriteit voor Voedselveiligheid met elkaar vergeleken. Zonder uitzondering zeggen de richtlijnen dat het beter is om de inname van toegevoegde suikers drastisch te beperken. Maar in de richtlijnen staat niet dat alle koolhydraten moeten worden vermeden. In het algemeen wordt aanbevolen om tot circa 50 procent koolhydraat te eten. Dr Brouns vindt dat de verhouding ook wel 40 - 60 procent zou kunnen zijn mits er sprake is van het kiezen van koolhydraatbronnen met een hoog vezelgehalte en vooral onverzadigde vetbronnen.
Dit zijn de kernpunten uit de richtlijnen:
- Elk type dieet dat mensen met overgewicht stimuleert om minder voedsel te eten en minder energie in te nemen, zal in eerste instantie leiden tot gewichtsverlies, wat op zichzelf tot gunstige metabole en functionele veranderingen zal leiden.
- De beschikbare wetenschappelijke literatuur laat zien dat gecontroleerde dieetstudies (enkele weken tot <2 jaar) met LCHF (koolhydraatarm dieet) bij personen met obesitas en diabetes gunstige effecten op gewichtsverlies, bloedglucose en insuline oplevert, maar ook enkele minder gewenste effecten (verhoging van LDL-cholesterol, afname vasculaire reactiviteit).
- Naleving van KLCHF-diëten lijkt moeilijk en na enige tijd lijken veel mensen toch weer over te gaan naar hogere innames van koolhydraten in volumes van 130-160 g / dag. Daarom kan het zich richten op 100-150 g / dag beter te zijn en makkelijker vol te houden.
- Er is gebrek aan gegevens die de werkzaamheid, veiligheid en gezondheidsvoordelen op lange termijn van LCHF-diëten ondersteunen. Elke aanbeveling moet in dit licht worden beoordeeld.
- Personen met diabetes-2 of borderline-diabetes worden aanbevolen om hun dagelijkse inname van snel verteerbare koolhydraten (suikers, siropen, aardappel, witte rijst, wit brood, enz.) te beperken. Daarnaast wordt aanbevolen dat mensen bij het overschakelen naar een dieet met een hoger vetgehalte voornamelijk producten kiezen die rijk zijn aan onverzadigde vetzuren.
- Leefstijlinterventies bij mensen met een hoog risico op het ontwikkelen van diabetes-2, met behoud van een relatief koolhydraatrijk dieet, resulteren in langdurige preventie van progressie tot diabetes-2 en deze dieëten worden over het algemeen als veilig gezien. Vanwege de complexiteit van de mogelijke mechanismen, hun interacties en de afwezigheid van gegevens uit goed gecontroleerde langetermijnstudies (> 2 jaar), lijkt het prematuur om een algemene openbare, op wetenschappelijk bewijs gebaseerde aanbeveling om KLCHF en LCHF te ondersteunen als een preventieve maatregel om de risico's te verminderen van diabetes-2. De rol van langdurig verhoogde vetconsumptie in combinatie met een laag koolhydraatconsumptie verdient nadere bestudering voordat algemene aanbevelingen kunnen worden gedaan.
Het volledige studierapport: Overweight and diabetes prevention: is a low-carbohydrate–high-fat diet recommendable? is gratis in te zien.
Hier het abstract van de studie met referentielijst.
Lifestyle intervention in people at high risk of developing type 2 diabetes, while maintaining a relative carbohydrate-rich diet, results in long-term prevention of progression to type 2 diabetes and is generally seen as safe.
Overweight and diabetes prevention: is a low-carbohydrate-high-fat diet recommendable?
Abstract
In the past, different types of diet with a generally low-carbohydrate content (< 50-< 20 g/day) have been promoted, for weight loss and diabetes, and the effectiveness of a very low dietary carbohydrate content has always been a matter of debate. A significant reduction in the amount of carbohydrates in the diet is usually accompanied by an increase in the amount of fat and to a lesser extent, also protein. Accordingly, using the term "low carb-high fat" (LCHF) diet is most appropriate. Low/very low intakes of carbohydrate food sources may impact on overall diet quality and long-term effects of such drastic diet changes remain at present unknown. This narrative review highlights recent metabolic and clinical outcomes of studies as well as practical feasibility of low LCHF diets. A few relevant observations are as follows: (1) any diet type resulting in reduced energy intake will result in weight loss and related favorable metabolic and functional changes; (2) short-term LCHF studies show both favorable and less desirable effects; (3) sustained adherence to a ketogenic LCHF diet appears to be difficult. A non-ketogenic diet supplying 100-150 g carbohydrate/day, under good control, may be more practical. (4) There is lack of data supporting long-term efficacy, safety and health benefits of LCHF diets. Any recommendation should be judged in this light. (5) Lifestyle intervention in people at high risk of developing type 2 diabetes, while maintaining a relative carbohydrate-rich diet, results in long-term prevention of progression to type 2 diabetes and is generally seen as safe.
References
-
1.Hauner H, Bechthold A, Boeing H, Brönstrup A, Buyken A, Leschik-Bonnet E, Linseisen J, Schulze M, Strohm D, Wolfram G (2012) Evidence-based guideline of the German Nutrition Society: carbohydrate intake and prevention of nutrition-related diseases. Ann Nutr Metab 60(Suppl. 1):1–58CrossRefGoogle Scholar
-
2.Gezondheidsraad (2015) Richtlijnen goede voeding 2015. http://www.erasmusage.com/wp-content/uploads/2015/11/201524_richtlijnen_goede_voeding_2015.pdf. Accessed May 2017
-
3.Nutrition SACo (2015) Carbohydrates and health. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/445503/SACN_Carbohydrates_and_Health.pdf. Accessed May 2017
-
4.World Health Organization (2015) Guideline: sugars intake for adults and children. World Health Organization. http://apps.who.int/iris/bitstream/10665/149782/1/9789241549028_eng.pdf. Accessed May 2017
-
5.World Health Organization (2015) Global status report on noncommunicable diseases, 2014: attaining the nine global noncommunicable diseases targets; a shared responsibility. World Health Organization, Geneva. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1. Accessed May 2017
-
6.Amine E, Baba N, Belhadj M, Deurenbery-Yap M, Djazayery A, Forrester T, Galuska D, Herman S, James W, MBuyamba J (2002) Diet, nutrition and the prevention of chronic diseases: report of a Joint WHO/FAO Expert Consultation. World Health Organization. http://www.who.int/dietphysicalactivity/publications/trs916/en/gsfao_introduction.pdf. Accessed May 2017
-
7.DeSalvo KB, Olson R, Casavale KO (2016) Dietary guidelines for Americans. JAMA 315(5):457–458CrossRefGoogle Scholar
-
8.Atkins RD (2002) Dr. Atkins’ new diet revolution. Government Institutes. https://shop.atkins.com/Books/c/Atkins@Books. Accessed May 2017
-
9.Sears B (1991) The zone diet. http://www.zonediet.com. Accessed May 2017
-
10.Agatston A (2001) The South Beach Diet. http://www.southbeachdiet.com. Accessed May 2017
-
11.Adam-Perrot A, Clifton P, Brouns F (2006) Low-carbohydrate diets: nutritional and physiological aspects. Obes Rev 7(1):49–58CrossRefGoogle Scholar
-
12.McDonald L (1998) The ketogenic diet: a complete guide for the dieter and practitioner. Lyle McDonald. http://biblioteca.usv.ro/Carti/Nutrition/The%20Ketogenic%20Diet-%20A%20Complete%20Guide%20For%20Practitioner%20McDonald%200-323x.pdf. Accessed May 2017
-
13.Volek JS, Fernandez ML, Feinman RD, Phinney SD (2008) Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog Lipid Res 47(5):307–318CrossRefGoogle Scholar
-
14.Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, Westman EC, Accurso A, Frassetto L, Gower BA, McFarlane SI (2015) Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 31(1):1–13CrossRefGoogle Scholar
-
15.Barnard ND, Scialli AR, Turner-McGrievy G, Lanou AJ, Glass J (2005) The effects of a low-fat, plant-based dietary intervention on body weight, metabolism, and insulin sensitivity. Am J Med 118(9):991–997CrossRefGoogle Scholar
-
16.Barnard ND, Cohen J, Jenkins DJ, Turner-McGrievy G, Gloede L, Jaster B, Seidl K, Green AA, Talpers S (2006) A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care 29(8):1777–1783CrossRefGoogle Scholar
-
17.Barnard ND, Gloede L, Cohen J, Jenkins DJ, Turner-McGrievy G, Green AA, Ferdowsian H (2009) A low-fat vegan diet elicits greater macronutrient changes, but is comparable in adherence and acceptability, compared with a more conventional diabetes diet among individuals with type 2 diabetes. J Am Diet Assoc 109(2):263–272CrossRefGoogle Scholar
-
18.Jenkins DJ, Kendall CW, Marchie A, Jenkins AL, Augustin LS, Ludwig DS, Barnard ND, Anderson JW (2003) Type 2 diabetes and the vegetarian diet. Am J Clin Nutr 78(3):610S–616SCrossRefGoogle Scholar
-
19.Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, Willett WC, Manson JE, Sun Q, Hu FB (2016) Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med 13(6):e1002039CrossRefGoogle Scholar
-
20.Huang R-Y, Huang C-C, Hu FB, Chavarro JE (2016) Vegetarian diets and weight reduction: a meta-analysis of randomized controlled trials. J Gen Intern Med 31(1):109–116CrossRefGoogle Scholar
-
21.Derbyshire EJ (2016) Flexitarian diets and health: a review of the evidence-based literature. Front Nutr 3:55. https://doi.org/10.3389/fnut.2016.00055 Google Scholar
-
22.Willcox DC, Scapagnini G, Willcox BJ (2014) Healthy aging diets other than the Mediterranean: a focus on the Okinawan diet. Mech Ageing Dev 136:148–162CrossRefGoogle Scholar
-
23.Noakes T (2014) Medical aspects of the low carbohydrate lifestyle. https://www.youtube.com/watch?v=fL5-9ZxamXc. Accessed May 2017
-
24.Eaton SB (2006) The ancestral human diet: what was it and should it be a paradigm for contemporary nutrition? Proc Nutr Soc 65(01):1–6CrossRefGoogle Scholar
-
25.Raubenheimer D, Rothman JM, Pontzer H, Simpson SJ (2014) Macronutrient contributions of insects to the diets of hunter–gatherers: a geometric analysis. J Hum Evol 71:70–76CrossRefGoogle Scholar
-
26.Eaton SB, Eaton SR, Konner MJ (1997) Paleolithic nutrition revisited: a twelve-year retrospective on its nature and implications. Eur J Clin Nutr 51(4):207–216CrossRefGoogle Scholar
-
27.Kaplan H, Thompson RC, Trumble BC, Wann LS, Allam AH, Beheim B, Frohlich B, Sutherland ML, Sutherland JD, Stieglitz J (2017) Coronary atherosclerosis in indigenous South American Tsimane: a cross-sectional cohort study. Lancet 389(10080):1730–1739CrossRefGoogle Scholar
-
28.Van Rossum C, Fransen H, Verkaik-Kloosterman J, Buurma-Rethans E, Ocké M (2011) Dutch National Food Consumption Survey 2007–2010: diet of children and adults aged 7 to 69 years. RIVM rapport 350050006Google Scholar
-
29.Westman EC, Feinman RD, Mavropoulos JC, Vernon MC, Volek JS, Wortman JA, Yancy WS, Phinney SD (2007) Low-carbohydrate nutrition and metabolism. Am J Clin Nutr 86(2):276–284CrossRefGoogle Scholar
-
30.VanItallie TB, Nufert TH (2003) Ketones: metabolism’s ugly duckling. Nutr Rev 61(10):327–341CrossRefGoogle Scholar
-
31.Wyk H, Davis R, Davies J (2016) A critical review of low-carbohydrate diets in people with type 2 diabetes. Diabet Med 33(2):148–157CrossRefGoogle Scholar
-
32.Hall K (2017) A review of the carbohydrate–insulin model of obesity. http://undark.org/wp-content/uploads/sites/2/2017/02/HallEJCN2017-1.pdf. Accessed May 2017
-
33.Vinuesa A, Pomilio C, Menafra M, Bonaventura MM, Garay L, Mercogliano MF, Schillaci R, Lantos VL, Brites F, Beauquis J (2016) Juvenile exposure to a high fat diet promotes behavioral and limbic alterations in the absence of obesity. Psychoneuroendocrinology 72:22–33CrossRefGoogle Scholar
-
34.Walker JM, Dixit S, Saulsberry AC, May JM, Harrison FE (2017) Reversal of high fat diet-induced obesity improves glucose tolerance, inflammatory response, β-amyloid accumulation and cognitive decline in the APP/PSEN1 mouse model of Alzheimer’s disease. Neurobiol Dis 100:87–98CrossRefGoogle Scholar
-
35.King M (2017) Gluconeogenesis: endogenous glucose synthesis. https://themedicalbiochemistrypage.org/gluconeogenesis.php. Accessed May 2017
-
36.Belkhou R, Cherel Y, Heitz A, Robin J-P, Le Maho Y (1991) Energy contribution of proteins and lipids during prolonged fasting in the rat. Nutr Res 11(4):365–374CrossRefGoogle Scholar
-
37.Rui L (2014) Energy metabolism in the liver. Compr Physiol 4(1):177–197. https://doi.org/10.1002/cphy.c130024 CrossRefGoogle Scholar
-
38.Yamazaki T, Okawa S, Takahashi M (2016) The effects on weight loss and gene expression in adipose and hepatic tissues of very-low carbohydrate and low-fat isoenergetic diets in diet-induced obese mice. Nutr Metab 13(1):78CrossRefGoogle Scholar
-
39.Accurso A, Bernstein RK, Dahlqvist A, Draznin B, Feinman RD, Fine EJ, Gleed A, Jacobs DB, Larson G, Lustig RH (2008) Dietary carbohydrate restriction in type 2 diabetes mellitus and metabolic syndrome: time for a critical appraisal. Nutr Metab 5(1):9CrossRefGoogle Scholar
-
40.Hu T, Mills KT, Yao L, Demanelis K, Eloustaz M, Yancy WS Jr, Kelly TN, He J, Bazzano LA (2012) Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am J Epidemiol 176(suppl_7):S44–SS54CrossRefGoogle Scholar
-
41.Kennedy ET, Bowman SA, Spence JT, Freedman M, King J (2001) Popular diets: correlation to health, nutrition, and obesity. J Acad Nutr Diet 101(4):411Google Scholar
-
42.U.S. Department of Agriculture ARS (1998) Data tables: food and nutrient intakes by region, 1994–96. http://www.barc.usda.gov/bhnrc/foodsurvey/home.htm. Accessed May 2017
-
43.Aune D, Keum N, Giovannucci E, Fadnes LT, Boffetta P, Greenwood DC, Tonstad S, Vatten LJ, Riboli E, Norat T (2016) Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ 353:i2716CrossRefGoogle Scholar
-
44.Ma X, Tang W-G, Yang Y, Zhang Q-L, Zheng J-L, Xiang Y-B (2016) Association between whole grain intake and all-cause mortality: a meta-analysis of cohort studies. Oncotarget 7(38):61996CrossRefGoogle Scholar
-
45.Albertson AM, Reicks M, Joshi N, Gugger CK (2016) Whole grain consumption trends and associations with body weight measures in the United States: results from the cross sectional National Health and Nutrition Examination Survey 2001–2012. Nutr J 15(1):8CrossRefGoogle Scholar
-
46.Vanegas SM, Meydani M, Barnett JB, Goldin B, Kane A, Rasmussen H, Brown C, Vangay P, Knights D, Jonnalagadda S (2017) Substituting whole grains for refined grains in a 6-wk randomized trial has a modest effect on gut microbiota and immune and inflammatory markers of healthy adults. Am J Clin Nutr 105(3):635–650CrossRefGoogle Scholar
-
47.Astrup A, Grunwald G, Melanson E, Saris W, Hill J (2000) The role of low-fat diets in body weight control: a meta-analysis of ad libitum dietary intervention studies. Int J Obes 24(12):1545CrossRefGoogle Scholar
-
48.Hall KD, Bemis T, Brychta R, Chen KY, Courville A, Crayner EJ, Goodwin S, Guo J, Howard L, Knuth ND (2015) Calorie for calorie, dietary fat restriction results in more body fat loss than carbohydrate restriction in people with obesity. Cell Metab 22(3):427–436CrossRefGoogle Scholar
-
49.Mansoor N, Vinknes KJ, Veierød MB, Retterstøl K (2016) Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr 115(03):466–479CrossRefGoogle Scholar
-
50.Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Brehm BJ, Bucher HC (2006) Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 166(3):285–293CrossRefGoogle Scholar
-
51.Wood TR, Hansen R, Sigurðsson AF, Jóhannsson GF (2016) The cardiovascular risk reduction benefits of a low-carbohydrate diet outweigh the potential increase in LDL-cholesterol. Br J Nutr 115(6):1126CrossRefGoogle Scholar
-
52.Buyken AE, Dussort DJM,P, Johnson IT, Macdonald IA, Stowell JD, Brouns FJPH. (2017) Dietary carbohydrates: a review of international recommendations and the methods used to derive them. Eur J Clin Nutr. https://doi.org/10.1038/s41430-017-0035-4. (in press)Google Scholar
-
53.Stern L, Iqbal N, Seshadri P, Chicano KL, Daily DA, McGrory J, Williams M, Gracely EJ, Samaha FF (2004) The effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trial. Ann Intern Med 140(10):778–785CrossRefGoogle Scholar
-
54.Foster GD, Wyatt HR, Hill JO, McGuckin BG, Brill C, Mohammed BS, Szapary PO, Rader DJ, Edman JS, Klein S (2003) A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 348(21):2082–2090CrossRefGoogle Scholar
-
55.Bradley U, Spence M, Courtney CH, McKinley MC, Ennis CN, McCance DR, McEneny J, Bell PM, Young IS, Hunter SJ (2009) Low-fat versus low-carbohydrate weight reduction diets. Diabetes 58(12):2741–2748CrossRefGoogle Scholar
-
56.Bilsborough SA, Crowe T (2003) Low carbohydrate diets: what are the potential short and long term health implications? Asia Pac J Clin Nutr 12(4):397–404Google Scholar
-
57.Brinkworth GD, Noakes M, Clifton PM, Bird AR (2009) Comparative effects of very low-carbohydrate, high-fat and high-carbohydrate, low-fat weight-loss diets on bowel habit and faecal short-chain fatty acids and bacterial populations. Br J Nutr 101(10):1493–1502CrossRefGoogle Scholar
-
58.Naude CE, Schoonees A, Senekal M, Young T, Garner P, Volmink J (2014) Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS One 9(7):e100652CrossRefGoogle Scholar
-
59.Dyson P (2015) Low carbohydrate diets and type 2 diabetes: what is the latest evidence? Diabetes Therapy 6(4):411–424CrossRefGoogle Scholar
-
60.Noto H, Goto A, Tsujimoto T, Noda M (2013) Low-carbohydrate diets and all-cause mortality: a systematic review and meta-analysis of observational studies. PLoS One 8(1):e55030CrossRefGoogle Scholar
-
61.Zilkha N, Kuperman Y, Kimchi T (2017) High-fat diet exacerbates cognitive rigidity and social deficiency in the BTBR mouse model of autism. Neuroscience 345:142–154CrossRefGoogle Scholar
-
62.Raider K, Ma D, Harris JL, Fuentes I, Rogers RS, Wheatley JL, Geiger PC, Yeh H-W, Choi I-Y, Brooks WM (2016) A high fat diet alters metabolic and bioenergetic function in the brain: a magnetic resonance spectroscopy study. Neurochem Int 97:172–180CrossRefGoogle Scholar
-
63.Del Rio D, Morales L, Ruiz-Gayo M, Del Olmo N (2016) Effect of high-fat diets on mood and learning performance in adolescent mice. Behav Brain Res 311:167–172CrossRefGoogle Scholar
-
64.Wang W, Yang J, Yang H, Sanidad KZ, Hammock BD, Kim D, Zhang G (2016) Effects of high-fat diet on plasma profiles of eicosanoid metabolites in mice. Prostaglandins Other Lipid Mediat 127:9–13CrossRefGoogle Scholar
-
65.Long Z, Zhang X, Sun Q, Liu Y, Liao N, Wu H, Wang X, Hai C (2017) Evolution of metabolic disorder in rats fed high sucrose or high fat diet: focus on redox state and mitochondrial function. Gen Comp Endocrinol 242:92–100. https://doi.org/10.1016/j.ygcen.2015.10.012 CrossRefGoogle Scholar
-
66.O’Neill AM, Burrington CM, Gillaspie EA, Lynch DT, Horsman MJ, Greene MW (2016) High-fat Western diet–induced obesity contributes to increased tumor growth in mouse models of human colon cancer. Nutr Res 36(12):1325–1334CrossRefGoogle Scholar
-
67.Moon C-M, Oh C-H, Ahn K-Y, Yang J-S, Kim J-Y, Shin S-S, Lim H-S, Heo S-H, Seon H-J, Kim J-W (2017) Metabolic biomarkers for non-alcoholic fatty liver disease induced by high-fat diet: In vivo magnetic resonance spectroscopy of hyperpolarized [1–13 C] pyruvate. Biochem Biophys Res Commun 482(1):112–119CrossRefGoogle Scholar
-
68.Kai M, Miyoshi M, Fujiwara M, Nishiyama Y, Inoue T, Maeshige N, Hamada Y, Usami M (2017) A lard-rich high-fat diet increases hepatic peroxisome proliferator-activated receptors in endotoxemic rats. J Surg Res 212:22–32CrossRefGoogle Scholar
-
69.Xia S, Lin R, Jin L, Zhao L, Kang HB, Pan Y, Liu S, Qian G, Qian Z, Konstantakou E, Zhang B, Dong JT, Chung YR, Abdel-Wahab O, Merghoub T, Zhou L, Kudchadkar RR, Lawson DH, Khoury HJ, Khuri FR, Boise LH, Lonial S, Lee BH, Pollack BP, Arbiser JL, Fan J, Lei QY, Chen J (2017) Prevention of dietary-fat-fueled ketogenesis attenuates BRAF V600E tumor growth. Cell Metab 25(2):358–373. https://doi.org/10.1016/j.cmet.2016.12.010 CrossRefGoogle Scholar
-
70.Yamasaki M, Hasegawa S, Imai M, Takahashi N, Fukui T (2016) High-fat diet-induced obesity stimulates ketone body utilization in osteoclasts of the mouse bone. Biochem Biophys Res Commun 473(2):654–661CrossRefGoogle Scholar
-
71.Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57(6):1470–1481. https://doi.org/10.2337/db07-1403 CrossRefGoogle Scholar
-
72.Martin K, Jackson CF, Levy RG, Cooper PN (2016) Ketogenic diet and other dietary treatments for epilepsy. Cochrane Database Syst Rev 2:CD001903. https://doi.org/10.1002/14651858.CD001903.pub3 Google Scholar
-
73.McKenzie M, Illingworth S (2017) Should a low carbohydrate diet be recommended for diabetes management? Proc Nutr Soc 76 (OCE1). https://doi.org/10.1017/S0029665117000192
-
74.Hjorth MF, Ritz C, Blaak EE, Saris WH, Langin D, Poulsen SK, Larsen TM, Sørensen TI, Zohar Y, Astrup A (2017) Pretreatment fasting plasma glucose and insulin modify dietary weight loss success: results from 3 randomized clinical trials. Am J Clin Nutr 106(2):499–505CrossRefGoogle Scholar
-
75.Astrup A, Hjorth MF (2017) Low-fat or low carb for weight loss? It depends on your glucose metabolism. EBioMedicine 22:20CrossRefGoogle Scholar
-
76.Snorgaard O, Poulsen GM, Andersen HK, Astrup A (2017) Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care 5(1):e000354CrossRefGoogle Scholar
-
77.Mithril C, Dragsted LO, Meyer C, Blauert E, Holt MK, Astrup A (2012) Guidelines for the new Nordic diet. Public Health Nutr 15(10):1941–1947CrossRefGoogle Scholar
-
78.Lindström J, Peltonen M, Eriksson J, Ilanne-Parikka P, Aunola S, Keinänen-Kiukaanniemi S, Uusitupa M, Tuomilehto J, Study FDP (2013) Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia 56(2):284–293CrossRefGoogle Scholar
-
79.Schellenberg ES, Dryden DM, Vandermeer B, Ha C, Korownyk C (2013) Lifestyle interventions for patients with and at risk for type 2 diabetes—a systematic review and meta-analysis. Ann Intern Med 159(8):543–551CrossRefGoogle Scholar
Copyright information
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Gerelateerde artikelen
- Algemeen: Voeding en voedingstoffen die een preventief effect hebben om kanker: te voorkomen. Een aantal studies en aanbevelingen bij elkaar gezet.
- ALS - amyotrofische laterale sclerose is via een bloedtest 10 jaar eerder te ontdekken voordat symptomen tot klachten gaan leiden
- Alzheimer - dementie is via een bloedtest jaren voordat de ziekte zich openbaart op te sporen en daardoor wellicht ook te voorkomen of uit te stellen voordat de ziekte ernstig wordt.
- Antibiotica speelt mogelijk rol bij ontstaan PDS - Prikkelbare Darm Syndroom.
- Asbest lijkt ook kanker in het strottenhoofd, maagkanker en darmkanker te kunnen veroorzaken.
- Aspirine ter voorkoming van kanker of een recidief van kanker: een overzicht van studies met aspirine copy 1
- Bacterien in de mond - Commensale microbiome en met name Genera Corynebacterium en Kingela spelen grote rol in wel of niet ontwikkelen van mond- en keelkanker. Vooral bij zware rokers en drinkers.
- Diakonessenhuis Utrecht biedt VEGA-Checker aan die bloedwaarden controleert of je lichaam wel alle vitamines en mineralen binnenkrijgt die het nodig heeft.
- DIM - diindolylmethane voorkomt voor 100 procent baarmoederhalskanker (100 procent vs 61 procent bij placebo) bij vrouwen met hoog risico door aanwezigheid van intraepithelial neoplasia (CIN I–II)
- Bloedbiomarker waarden van CRP, LDL cholesterol en lipoproteïne (a), kunnen vrouwen tientallen jaren van tevoren een beeld geven van hun risico op hartziekten
- Bloedtest die methyl meet in cellen kan ruim van te voren voorspellen of iemand borstkanker gaat ontwikkelen. Blijkt uit jarenlang onderzoek. copy 1
- Baarmoederhalskanker veel beter - 60 procent - te voorkomen door DNA test op het HPV virus in vergelijking met uitstrijkje
- Baarmoederkanker is te voorkomen (tot 40 procent) met veel bewegen en stabiel lichaamsgewicht. Te dik geeft meer risico op baarmoederkanker.
- Bewegen: Mensen die te weinig bewegen en zittend hun dagen doorbrengen hadden 82 procent hoger risico om te overlijden aan kanker vergeleken met mensen die veel bewegen en sporten, zelfs na correctie voor leeftijd, geslacht en ziektestatus.
- Bovine Lactoferrin (bLF) stimuleert het immuunsysteem en remt groei darmpoliepen, aldus dubbelblinde gerandomiseerde studie.
- Borstkanker - preventie: een overzicht van belangrijke artikelen en recente studies hoe het risico op borstkanker te verkleinen
- BRCA-1 mutatie verdubbelt risico op baarmoederkanker bij vrouwen met BRCA-1 gen en 26x grotere kans in vergelijking met vrouwen zonder BRCA mutaties
- Cardiovasculaire risicofactoren: Hoe meer cardiovasculaire risicofactoren iemand had als kind en tiener - zoals obesitas, hoge bloeddruk en hoog cholesterolgehalte - hoe lager ze presteerden op geheugen- en denktesten na hun dertigste en 40e.
- Cardiorespiratoire fitheid verbeteren door sporten en bewegen kan ontstaan van prostaatkanker verminderen, blijkt uit Zweedse studie bij circa 50000 mannen
- Chemo en bestraling voor kinderen met kanker vergroot 6 tot 13 keer het risico op krijgen van borstkanker voor hun 40e jaar in vergelijking met bevolkingsrisico.
- Darmbarriere speelt een centrale rol in onze gezondheid. Verstoringen zorgen voor een groter risico op stofwisselingsziektes en speelt ook grote rol in immuniteit.
- Microbioom - Darmflora, een aantal artikelen bij elkaar gezet
- Darmkanker: Een periodieke colonoscopie - inwendig darmonderzoek - vermindert het risico op darmkanker stadium IIB of hoger met 70%.
- Depressie en angst leiden niet tot meer vormen van kanker blijkt uit jarenlang internationaal onderzoek
- Diabetes: Harmine, een natuurlijke alkaloide, blijkt de insuline productie te herstellen bij diabetes patienten en lijkt uitstekende behandeling om diabetes 1 en 2 te genezen
- Diagnostische fouten komen vaak voor in ziekenhuizen. 1 op de 14 patienten krijgt verkeerde diagnose maar is heel vaak te voorkomen.
- Gordelroosvaccin verlaagt risico met meer dan 20 procent op hart- en vaatziekten en blijft actief beschermen tot wel acht jaar na eerste vaccinatie
- Het Kytogeen dieet - koolhydraatarm dieet - strikt volgen kan schadelijk zijn. Lage hoeveelheid vezels en hoog vetgehalte leidt tot onevenwichtige darmflora.
- Hormoontherapie na de menopauze kan risico op kanker verhogen of verkleinen. Oestrogeen verhoogt. Oestrogeen plus Progesteen verkleint.
- HST - Hormoontherapie in en tijdens de overgang veroorzaakt 54 tot 93% kans op galwegziekte, aldus dubbelblinde gerandomiseerde studie bij ruim 14.000 gezonde vrouwen
- Infecties veroorzaken 16 procent van alle vormen van kanker wereldwijd. Leefstijl plus infecties zou voor 35 procent verantwoordelijk zijn aldus grote epidemologische studie in 184 landen
- Leefstijl en voeding in eerste twintig jaar van een mensenleven lijkt bepalend voor risico op krijgen van kanker toont grote Zweedse studie.
- Longkanker: Rauwe knoflook zou de kans op longkanker (44 procent) sterk verminderen. Blijkt uit groot Chinees onderzoek
- Mobiele telefoons geven verhoogd risico op kanker bij kinderen
- Nieuwe richtlijn ‘Overgewicht en obesitas bij volwassenen’ waarbij meetlint de weegschaal vervangt
- NIPT = Niet Invasieve Prenatale celvrije DNA-Test die geen resultaat laat zien of abnormale data betekent vaak (52 procent) dat de moeder beginnende kanker heeft blijkt uit de IDENTIFY studie
- Paddenstoelen: hogere dagelijkse consumptie van paddenstoelen geeft minder risico op krijgen van kanker. Verschil kan oplopen tot 47 procent.
- Parkinson: Aantal patienten met ziekte van Parkinson is schrikbarend gegroeit, vooral door milieuvervuiling als fijnstof en landbouwgif die worden gebruikt in de landbouw en tuinbouw
- PFAS producten lijken groter risico te geven op vormen van hormoongerelateerde kanker bij vrouwen, zoals eierstokkanker maar ook op een melanoom
- Ploegendienst met nachtdiensten vergroot de kans op het ontwikkelen van eierstokkanker
- Probiotica - melkzuurbacteriën kunnen in veel gevallen ziektes voorkomen of zorgen voor herstel van darmflora na chemo of bestraling
- Prostaatkanker: Dieet met groenten, fruit, vis, peulvruchten en volkoren granen vermindert duidelijk de kans op overlijden aan niet uitgezaaide prostaatkanker bij diagnose in vergelijking met westers dieet copy 1
- Psycho stimulerende middelen zoals Ritalin aan kinderen geeft verhoogde kans op krijgen van kanker later. Na 3 maanden ontstond een ernstige chromosoom afwijking. Fase III studie toegevoegd naar effecten van psycho stimulerende middelen op gezondheid
- ReCET - electroporation therapy is een nieuwe endoscopische behandeling en verbetert glykemische controle en stopt behoefte aan medisch toepassen van insuline bij patiënten met diabetes type 2
- Roken is nog schadelijker dan gedacht, maar stoppen met roken kan ook je leven verlengen.
- Screening: Draagbaar ultrasound scanapparaat blijkt uitstekende resultaten te geven bij ontdekken van kwaadaardige tumoren bij mensen met hoog risico op ontwikkelen van borstkanker
- Screeningtesten voor opsporen van kanker zoals voor borstkanker, longkanker, darmkanker en prostaatkanker lijken geen invloed te hebben op uiteindelijke levensduur
- Slaapmiddelen die regelmatig worden gebruikt door volwassenen zouden een 3 keer zo hoog risico geven eerder te sterven en meer kans op kanker in vergelijking met zelden of nooit slaapmiddelen gebruik
- Sociale stress zoals discriminatie en gezinsproblemen, samen met werk- en geldproblemen, kunnen bijdragen aan vroegtijdige veroudering van menselijk immuunsysteem
- Testosteronwaarde is sterk gerelateerd aan botdichtheidsverlies Bijna de helft van de mannen met een laag testosteron had osteopenie of osteoporose.
- Uromune vaccin is bijzonder effectief voor patiënten met recidiverende urineweginfecties (rUTI). 54 procent bleef 9 jaar gevrijwaard van een urineweginfectie zonder gebruik van antibiotica
- Vibratorgebruik kan de bekkengezondheid verbeteren bij vrouwen. Vibratorgebruik verbetert seksuele gezondheid, urine-incontinentie en vulvaire pijn
- Algemene informatie preventie



Plaats een reactie ...
Reageer op "Het Kytogeen dieet - koolhydraatarm dieet - strikt volgen kan schadelijk zijn. Lage hoeveelheid vezels en hoog vetgehalte leidt tot onevenwichtige darmflora."