Helpt u ons aan 500 donateurs?
15 mei 2018: zie ook dit artikel:
https://kanker-actueel.nl/synbiotica-vooraf-en-na-operatie-van-darmkanker-voorkomt-bijna-volledig-post-operatieve-infecties-in-vergelijking-met-placebo-1-vs-9-uit-90-patienten.html
1 oktober 2017: Bron: Gastroenterol Res Pract. 2017; 2017: 6029075 en Ann Gastroenterol. 2017; 30(1): 45–53
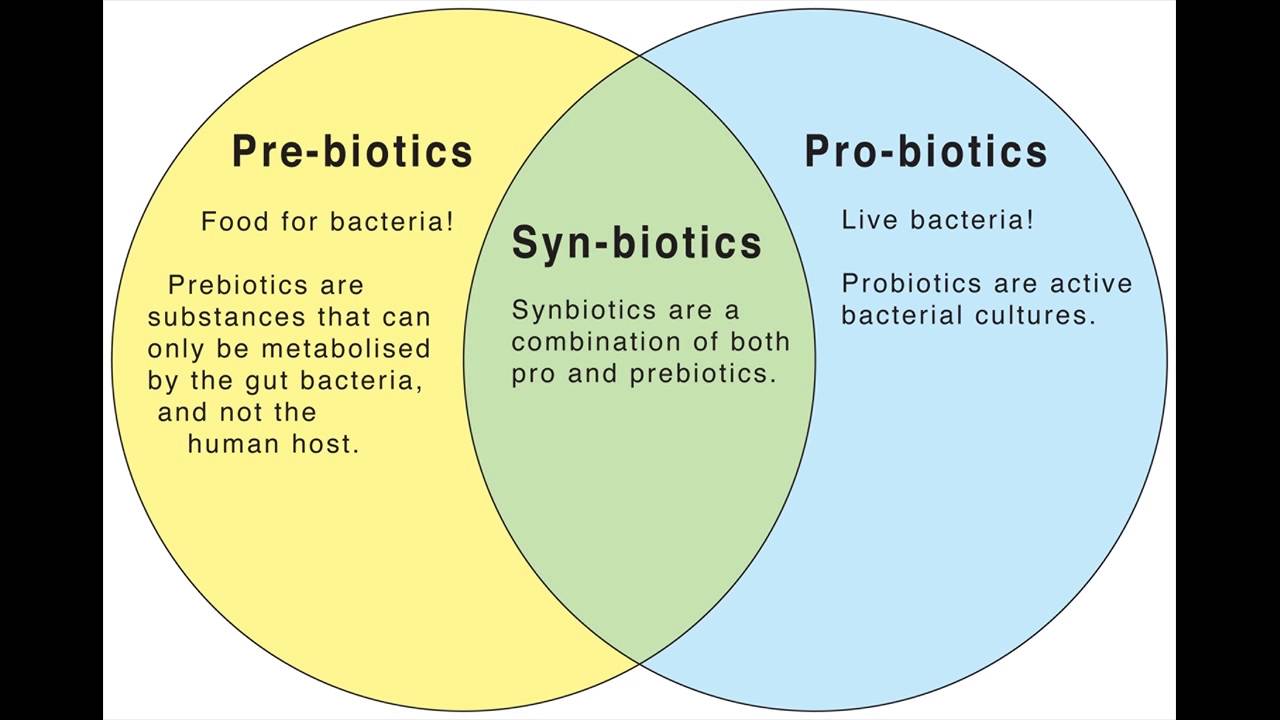
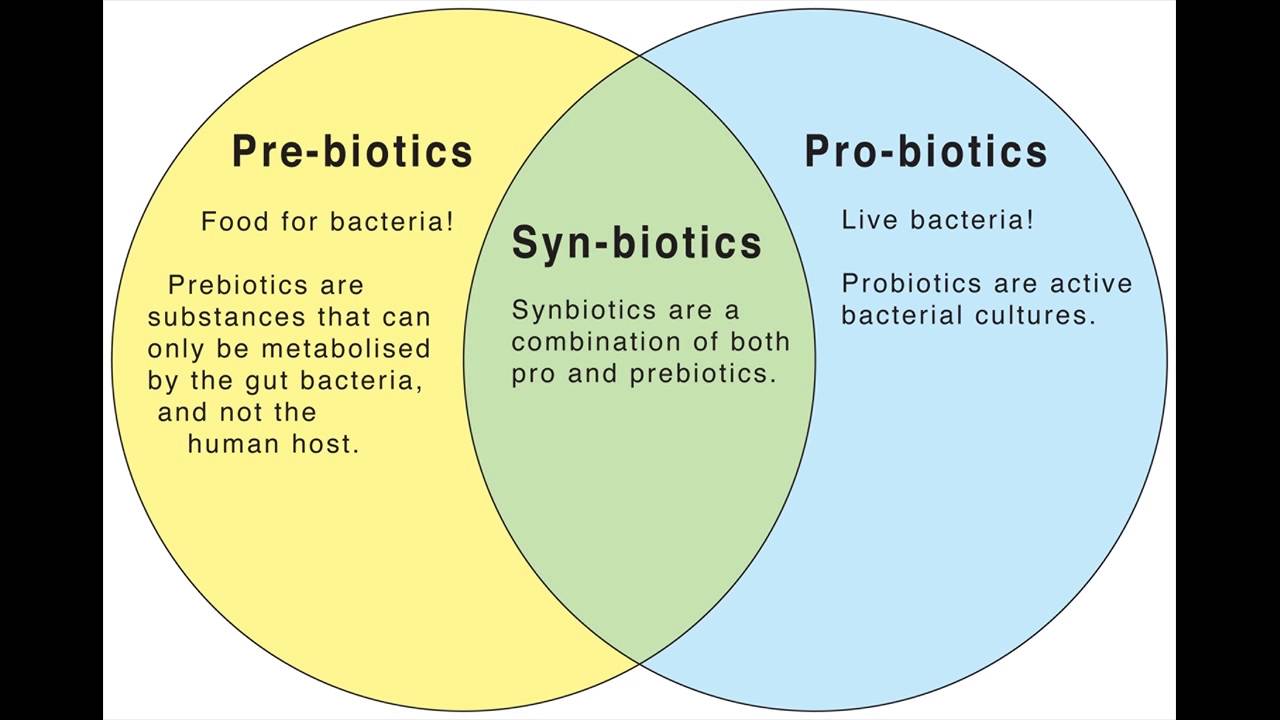
Zoals te zien is in gerelateerde artikelen hebben melkzuurbacteriën - probiotica heel vaak een gunstige invloed in vele opzichten en bij verschillende aandoeningen, ook gerelateerd aan kanker. Zo ook zijn er al verschillende studies gepubliceerd die bewijzen dat als patiënten met darmkanker vooraf en na een operatie bepaalde samenstellingen van melkzuurbacteriën / probiotica krijgen deze patiënten veel minder ernstige infecties krijgen en vaal sneller hun darmfunctie weer hersteld. En zijn de dagen dat ze in het ziekenhuis moeten blijven meestal korter in vergelijking met patiënten die geen melkzuurbacteriën / probiotica hebben gekregen / genomen. Wat niet eenduidig is is welke samenstellingen van melkzuurbacteriën - probiotica het beste effect hebben. Er zijn wereldwijd een aantal bedrijven die melkzuurbacteriën kweken en produceren en leveren aan bedrijven die leveren aan artsen en burgers. Het is dus altijd aan te raden om een deskundig arts of voedingsdeskundige te raadplegen wanneer u melkzuurbacteriën / probiotica wilt gaan gebruiken om welke reden dan ook.
Terug naar darmkanker en probiotica / melkzuurbacteriën.
Recent zijn twee reviewstudies gepubliceerd waarin een overzicht wordt gegeven van de effecten van melkzuurbacteriën / probiotica bij darmkanker operaties.
In deze meta-analyse van 9 gerandomiseerde studies: Probiotics Reduce Postoperative Infections in Patients Undergoing Colorectal Surgery: A Systematic Review and Meta-Analysis wordt een sterk effect gezien op het voorkomen van ernstige infecties en herstel na een operatie:
Table 2
Summary estimates and 95%CIs for total effects of the probiotics.
| Outcomes | Number of studies | Case | OR (95%CIs) | Z-test (p value) | χ 2 | HG∗p value |
|---|
| Probiotics | Placebo |
|---|
| Total infections |
5 |
397 |
417 |
0.59 [0.43, 0.83] |
0.002 |
7.11 |
0.13 |
| Surgical site infection (SSI) |
|
805 |
850 |
0.67 [0.49, 0.93] |
0.02 |
8.53 |
0.67 |
| Incision infection |
7 |
472 |
491 |
0.61 [0.41, 0.91] |
0.02 |
4.59 |
0.60 |
| Organ/space SSI |
4 |
333 |
359 |
0.82 [0.47, 1.42] |
0.48 |
3.15 |
0.53 |
| Nonsurgical site infection (NSSI) |
|
592 |
587 |
0.36 [0.23, 0.57] |
0.00001 |
6.26 |
0.79 |
| Urinary tract infection |
3 |
174 |
173 |
0.39 [0.16, 0.96] |
0.04 |
2.06 |
0.36 |
| Pneumonia |
4 |
209 |
207 |
0.25 [0.11, 0.60] |
0.002 |
0.47 |
0.92 |
| Bacteremia |
4 |
209 |
207 |
0.44 [0.23, 0.85] |
0.01 |
2.59 |
0.46 |
| Bacterial translocation |
2 |
95 |
97 |
0.13 [0.01, 1.48] |
0.10 |
6.28 |
0.01† |
| Anastomotic leakage |
4 |
382 |
399 |
0.80 [0.28, 2.48] |
0.70 |
7.08 |
0.07‡ |
∗HG: heterogeneity, χ2 test with a p value < 0.10 indicated significant heterogeneity across studies; †,‡there was obvious statistical heterogeneity, but no observed clinical heterogeneity, and a random effects model was adopted
En in deze studie: Gut microbiome, surgical complications and probiotics. zien de onderzoekers dat naast de positieve effecten bij een operatie ook het reinigen van de darmen en herstellen van de darmflora na bv antibiotica of morfine betere resultaten met melkzuurbacteriën / probiotica worden bereikt in het herstellen van de darmflora:
Figure 3
Effects of mechanical bowel cleansing on the intestinal microbiota
Uit dit laatste studierapport:
een recente meta-analyse toonde een vermindering van postoperatieve sepsis na algemene chirurgie, zowel bij pro- en synbiotisch behandelde patiënten in vergelijking met placebo (respectievelijk P = 0,003 en 0,002). Er is echter geen significant verschil gevonden in de incidentie van pneumonie, urineweginfecties of chirurgische plaatselijke infecties , terwijl in een recent gepubliceerde studie een significante daling van 38% bij de incidentie van postoperatieve sepsis bleek.
Een afzonderlijke analyse gerelateerd aan het type operatie toonde een statistisch significant verschil tussen de verschillende typen van chirurgie, met een 35% risico vermindering in darmkanker chirurgie, 73% bij leverkanker en alvleesklierkanker operaties en een 56% risico vermindering bij levertransplantaties; Deze bevindingen tonen aan dat patiënten met chirurgie van darmkanker de moeilijkste groep zijn voor de manipulatie van de darmmicrobiële balans. [zie onderaan referentie 80].
In deze studie: Probiotics and synbiotics for the prevention of postoperative infections following abdominal surgery: a systematic review and meta-analysis of randomized controlled trials.
bleek een infectie op de plaats van de operatie bij 6.8% voor te komen bij patiënten die wel extra melkzuurbacteriën hadden gekregen tegenover 11.1% in de controlegroep. Dit blijkt een risicovermindering te geven van 37 procent. Deze studie onderstreepte ook het potentiële voordeel in relatie tot urineweginfecties en samengestelde infecties, evenals het niet voorkomen van ernstige bijwerkingen die verband houden met de gebruikte melkzuurbacteriën, aldus de onderzoekers.
In onze literatuurlijst specifiek bij darmkanker worden een aantal studies vermeld onder het kopje probiotica / synbiotica / melkzuurbacteriën. Als u klikt op de studieomschrijving komt u bij de studierapporten. Inclusief die ik hierboven al heb genoemd.
Onder de studievermeldingen de referentielijsten behorend bij de eerste twee genoemde studies en het abstract van de meest recente studie onderaan dit lijstje:
Probiotica en synbiotica - melkzuurbacteriën:
Lees ook dit studierapport een meta-analyse van 9 gerandomiseerde studies: Probiotics Reduce Postoperative Infections in Patients Undergoing Colorectal Surgery: A Systematic Review and Meta-Analysis
en deze studie: Gut microbiome, surgical complications and probiotics.
168) Isenberg J et al ; Anticancer Res 15 : 2363-8 ; 1995 ; Propionibacterium avidum KP-40 verbetert in gerandomiseerd onderzoek in stadium 1 en 2 de overleving van patienten met darmkanker ; ook verbeterde het de levenskwaliteit.
273) Isenberg J et al ; Anticancer Res 14 : 1399-404 ; 1994 ; Propionibacterium granulosum vermindert bij operatie wegens darmkanker het aantal infecties en verbetert in stadium 1 en 2 de overleving ; echter niet in stadium 3 of 4. Een analyse met een chikwadraattoets van alle stadia bij elkaar zou evenwel zinvol zijn ; zie ook 275.
275) Grundmann R et al ; Chirurg 59 : 272-8 ; 1988 ; Propionibacterium granulosum vermindert bij patienten, die geopereerd worden wegens darmkanker het aantal infecties en het daar aan gerelateerde aantal nieuwe operaties ; de recidiefkans en de overleving werden in dit onderzoek door deze bacterie evenwel niet beinvloed. Propionibacterium granulosum komt er dus goed af ; zie naast deze publicatie ook 213, 273 en 274.
1229) Henriksson R et al ; Support Care Cancer 3: 81-3 ; 1995 ; Probioticum vermindert bij patienten die wegens kanker in de buik bestraald worden de darmklachten in vergelijking met een gerandomiseerde controle-groep. PMID 7697308. Zie ook 133 en 304, met vergelijkbare resultaten.
1366)Osterlund P et al ; Br J Cancer 97: 1028-34 ; 2007 ; Probiotica verminderen wel, vezels niet de bijwerkingen van 5-FU op de darm ; PMID 17895895 ; zie ook PMID 15290663
1378)Delia P et al ; World J Gastroenterol 13: 912-5 ; 2007 : Het probioticum VSL#3 vermindert in vergelijking met placebo aantoonbaar de met bestraling samenhangende diarree ; zie PMID 17352022 ; zie ook 304 en 1229, beide met een vergelijkbaar resultaat.
1445) Giralt J et al ; Int J Radiat Oncol Biol Phys 2008 Feb 1 (Epub ahead of print) ; Probioticum vermindert ernst diarree door bestraling ; zie de 3 eerdere studies in deze lijst met een vergelijkbaar resultaat ; PMID 18243569.
1611)Liu Y et al ; Di Yi Jun Yi Da Xue Xue Bao 2005 Oct;25(10):1308-11; PMID 16234118 ; Lactone I van Atractyloides macrocephala Koidz bleek bij cachectische kankerpatienten in vergelijking met een visoliesupplement de eetlust te verbeteren.
1625)Liu Z et al ; Aliment Pharmacol Ther 2011 Jan;33 (1):50-63;PMID 21083585 ; Probiotica verminderden in dit gerandomiseerd dubbelblind onderzoek de kans op infectie samenhangend met operatie wegens darmkanker!
1626)Horvat M et al ; Wien Klin Wochenschr. 2010 May;122 Suppl 2:26-30;PMID 20517667 ; Prebiotische reiniging darm even effectief als met een bekende mechanische reiniging van de darm om complicaties wegens colorectale chirurgie tegen te gaan.
1632)Watanabe M et al ; Br j Surg 2010 Dec;97(12):1791-7;PMID 20799286 ; mechanische darmreiniging vanwege een komende operatie wegens darmkanker vermindert zowel het aantal Lactobacillen als de Bifidobacterien in de darm ; dit lijkt zeker geen extra voordeel ; zie ook 1626.
1786)Liu ZH et al; Am J Clin Nutr 2013; Jan;97(1):117-26;PMID 23235200 ; Probiotische behandeling vermindert bij operatie wegens darmkanker de kans op postoperatieve infecties.
1870)Zhang JW et al; Am J Med Sci 2012 Mar;343(3):199-205;PMID22197980; Probiotica verminderen bij patiënten geopereerd voor darmkanker in vergelijking met placebo significant de kans op postoperatieve infecties.
2117)Zhang JW et al ; Zhonghua Wei Chang Wai Ke Za Zhi 2010 Jan;13(1):40-3;PMID 20099160; Bifidobacterium vermindert de kans op complicaties in verband met operatie wegens darmkanker.
2122)Can G et al; Oncol Nurs Forum 2009 Nov;36(6):E335-42;PMID19887347 : Kefir verminderde in dit onderzoek bij darmkankerpatienten niet de direkte bijwerkingen van de chemo, maar verminderde wel de slaapstoornissen.
2151)Garcia-Peris P et al; Nutr Hosp 2012 Nov-Dec;27(6):1908-15;PMID23588438 ; inuline plus oligofructose als prebioticum voor expliciet Lactobacilli en Bifidobacteria, bevordert het herstel van deze bacterien na radiotherapie ; zeer relevant, want dit soort bacterien gaan op zichzelf de bijwerkingen van radiotherapie voor de onderbuik tegen.
2288)Sadahiro S et al; Surgery 2014 Mar ;155(3):493-503:PMID 24524389 ; Probiotica verlagen na operatie voor darmkanker de infectiekans niet ; antibiotica doen dat wel.
2494)Lee JY et al ; Dig Liver Dis. 2014 Dec;46(12):1126-32;PMID 25442120 ; Probiotica verbeteren bij darmkankerpatienten de levenskwaliteit.
2508)Obigashi S et al; Surg Today 2011 Sep;41(9):1200-6; PMID 21874415 : Probioticum verbetert levenskwaliteit na operatie wegens darmkanker.
2557)Kotzampassi K et al ; World J Surg 2015 Apr 17; Probiotica verminderen postoperatieve complicaties darmkankerchirurgie.
2583)Shao F et al; Zhonghua Wei Chang Wai Ke Za Zhi 2012 May;15(5):476-9; Probioticum verbetert bij patienten met diabetes die voor darmkanker geopereerd moeten worden de diabetes zodanig, dat ze sneller van de operatie herstellen. PMID22648843
2717)Mego M et al ; Complement Ther Med 2015 Jun;23(3):356-62 ; PMID26051570 ; Probioticum vermindert diarree bij gebruik irinotecan.
2751)Theodoropoulos GE et al ; 2016 Jam-March;29(1):56-62;PMID 26752951; een synbioticum verbetert de levenskwaliteit na operatie wegens darmkanker.
2758)Yang Y et al ; Oncotarget 2016 Jan 27; PMID 26824990 ; Bij operatie wegens darmkanker bevorderde probiotica het weer op gang komen van de stoelgang ; infecties etc. traden in de probiotica-groep niet significant minder op.
2985)Krebs B et al; Coll Antropol 2016 Apr;40(1):35-40;PMID 27301235 ; Pre- noch synbioticum preoperatief hadden invloed op ligduur, aantal complicaties etc. vanwege operatie aan darmkanker.
3222)Mizuta M et al; Biosci Microbiota Food Health 2016;35(2):77-87 ; PMID 2720026 ; Bifidobacteria bevorderde bij geopereerde kankerpatienten die chemoradiatie vooraf hadden gehad het herstel.
Het abstract van no. 3222:
Our findings suggest that the administration of B. longum BB536 may represent an effective strategy to maintain a balance in the microbiota and promote healthy recovery in patients undergoing surgery.
Perioperative supplementation with bifidobacteria improves postoperative nutritional recovery, inflammatory response, and fecal microbiota in patients undergoing colorectal surgery: a prospective, randomized clinical trial
Minoru MIZUTA,
1 Izuru ENDO,
1 Sumiharu YAMAMOTO,
1 Hidetoshi INOKAWA,
1 Masatoshi KUBO,
1 Tetsunobu UDAKA,
1 Osanori SOGABE,
1 Hiroya MAEDA,
1 Kazutoyo SHIRAKAWA,
1 Eriko OKAZAKI,
2 Toshitaka ODAMAKI,
3 Fumiaki ABE,
4 and
Jin-zhong XIAO3,*
This article has been
cited by other articles in PMC.
Abstract
The use of probiotics has been widely documented to benefit human health, but their clinical value in surgical patients remains unclear. The present study investigated the effect of perioperative oral administration of probiotic bifidobacteria to patients undergoing colorectal surgery. Sixty patients undergoing colorectal resection were randomized to two groups prior to resection. One group (n=31) received a probiotic supplement, Bifidobacterium longum BB536, preoperatively for 7–14 days and postoperatively for 14 days, while the other group (n=29) received no intervention as a control. The occurrences of postoperative infectious complications were recorded. Blood and fecal samples were collected before and after surgery. No significant difference was found in the incidence of postoperative infectious complications and duration of hospital stay between the two groups. In comparison to the control group, the probiotic group tended to have higher postoperative levels of erythrocytes, hemoglobin, lymphocytes, total protein, and albumin and lower levels of high sensitive C-reactive proteins. Postoperatively, the proportions of fecal bacteria changed significantly; Actinobacteria increased in the probiotic group, Bacteroidetes and Proteobacteria increased in the control group, and Firmicutes decreased in both groups. Significant correlations were found between the proportions of fecal bacteria and blood parameters; Actinobacteria correlated negatively with blood inflammatory parameters, while Bacteroidetes and Proteobacteria correlated positively with blood inflammatory parameters. In the subgroup of patients who received preoperative chemoradiotherapy treatment, the duration of hospital stay was significantly shortened upon probiotic intervention. These results suggest that perioperative oral administration of bifidobacteria may contribute to a balanced intestinal microbiota and attenuated postoperative inflammatory responses, which may subsequently promote a healthy recovery after colorectal resection.
Referenties behorend bij Gut microbiome, surgical complications and probiotics
References
1.
Alverdy J, Holbrook C, Rocha F, et al. Gut-derived sepsis occurs when the right pathogen with the right virulence genes meets the right host: evidence for in vivo virulence expression in Pseudomonas aeruginosa. Ann Surg. 2000;232:480–489. [PMC free article] [PubMed]2.
Rasid O, Cavaillon JM. Recent developments in severe sepsis research: from bench to bedside and back. Future Microbiol. 2016;11:293–314. [PubMed]3.
Shimizu K, Ogura H, Hamasaki T, et al. Altered gut flora are associated with septic complications and death in critically ill patients with systemic inflammatory response syndrome. Dig Dis Sci. 2011;56:1171–1177. [PMC free article] [PubMed]4.
Morowitz MJ, Babrowski T, Carlisle EM, et al. The human microbiome and surgical disease. Ann Surg. 2011;253:1094–1101. [PMC free article] [PubMed]5.
Zaborin A, Smith D, Garfield K, et al. Membership and behavior of ultra-low-diversity pathogen communities present in the gut of humans during prolonged critical illness. MBio. 2014;5:e01361–e01414. [PMC free article] [PubMed]6.
Claesson MJ, Jeffery IB, Conde S, et al. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488:178–184. [PubMed]7.
Kotzampassi K, Giamarellos-Bourboulis EJ. Probiotics for infectious diseases: more drugs, less dietary supplementation. Int J Antimicrob Agents. 2012;40:288–296. [PubMed]8.
Khanna S, Tosh PK. “A clinician’s primer on the role of the microbiome in human health and disease. Mayo Clin Proc. 2014;89:107–114. [PubMed]9.
Qin J, Li R, Raes J, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464:59–65. [PMC free article] [PubMed]10.
Eckburg PB, Bik EM, Bernstein CN, et al. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–1638. [PMC free article] [PubMed]11.
Linares DM, Ross P, Stanton C. Beneficial microbes: The pharmacy in the gut. Bioengineered. 2016;7:11–20. [PMC free article] [PubMed]12.
Francino MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol. 2016;6:1543. [PMC free article] [PubMed]13.
Shimizu K, Ogura H, Goto M, et al. Altered gut flora and environment in patients with severe SIRS. J Trauma. 2006;60:126–133. [PubMed]14.
Eleftheriadis E, Kotzampassi K, Papanotas K, Heliadis N, Sarris K. Gut ischemia, oxidative stress, and bacterial translocation in elevated abdominal pressure in rats. World J Surg. 1996;20:11–16. [PubMed]15.
Lapthorne S, Bines JE, Fouhy F, et al. Changes in the colon microbiota and intestinal cytokine gene expression following minimal intestinal surgery. World J Gastroenterol. 2015;21:4150–4158. [PMC free article] [PubMed]16.
Watanabe M, Murakami M, Nakao K, Asahara T, Nomoto K, Tsunoda A. Randomized clinical trial of the influence of mechanical bowel preparation on faecal microflora in patients undergoing colonic cancer resection. Br J Surg. 2010;97:1791–1797. [PubMed]17.
Fry DE. Colon preparation and surgical site infection. Am J Surg. 2011;202:225–232. [PubMed]18.
Slim K, Vicaut E, Launay-Savary MV, Contant C, Chipponi J. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery. Ann Surg. 2009;249:203–209. [PubMed]19.
Güenaga KF, Matos D, Wille-Jørgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev. 2011;9:CD001544. [PubMed]20.
Harrell L, Wang Y, Antonopoulos D, et al. Standard colonic lavage alters the natural state of mucosal-associated microbiota in the human colon. PLoS One. 2012;7:e32545. [PMC free article] [PubMed]21.
Ringel Y, Maharshak N, Ringel-Kulka T, Wolber EA, Sartor RB, Carroll IM. High throughput sequencing reveals distinct microbial populations within the mucosal and luminal niches in healthy individuals. Gut Microbes. 2015;6:173–181. [PMC free article] [PubMed]22.
Jalanka J, Salonen A, Salojärvi J, et al. Effects of bowel cleansing on the intestinal microbiota. Gut. 2015;64:1562–1568. [PubMed]23.
Drago L, Toscano M, De Grandi R, Casini V, Pace F. Persisting changes of intestinal microbiota after bowel lavage and colonoscopy. Eur J Gastroenterol Hepatol. 2016;28:532–537. [PubMed]24.
Wexner SD, Beck DE, Baron TH, et al. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Gastrointest Endosc. 2006;63:894–909. [PubMed]25.
Strocchi A, Bond JH, Ellis C, Levitt MD. Colonic concentrations of hydrogen and methane following colonoscopic preparation with an oral lavage solution. Gastrointest Endosc. 1990;36:580–582. [PubMed]26.
Johansson ME, Gustafsson JK, Holmén-Larsson J, et al. Bacteria penetrate the normally impenetrable inner colon mucus layer in both murine colitis models and patients with ulcerative colitis. Gut. 2014;63:281–291. [PMC free article] [PubMed]27.
Gayer CP, Basson MD. The effects of mechanical forces on intestinal physiology and pathology. Cell Signal. 2009;21:1237–1244. [PMC free article] [PubMed]28.
Cotter PD, Stanton C, Ross RP, Hill C. The impact of antibiotics on the gut microbiota as revealed by high throughput DNA sequencing. Discov Med. 2012;13:193–199. [PubMed]29.
Macfarlane S. Antibiotic treatments and microbes in the gut. Environ Microbiol. 2014;16:919–924. [PubMed]30.
Antunes LC, Han J, Ferreira RB, Lolić P, Borchers CH, Finlay BB. Effect of antibiotic treatment on the intestinal metabolome. Antimicrob Agents Chemother. 2011;55:1494–1503. [PMC free article] [PubMed]31.
Dethlefsen L, Huse S, Sogin ML, Relman DA. The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol. 2008;6:e280. [PMC free article] [PubMed]32.
Panda S, El khader I, Casellas F, et al. Short-term effect of antibiotics on human gut microbiota. PLoS One. 2014;9:e95476. [PMC free article] [PubMed]33.
Young VB, Schmidt TM. Antibiotic-associated diarrhea accompanied by large-scale alterations in the composition of the fecal microbiota. J Clin Microbiol. 2004;42:1203–1206. [PMC free article] [PubMed]34.
De La Cochetière MF, Durand T, Lepage P, Bourreille A, Galmiche JP, Doré J. Resilience of the dominant human fecal microbiota upon short-course antibiotic challenge. J Clin Microbiol. 2005;43:5588–5592. [PMC free article] [PubMed]35.
Donskey CJ, Hujer AM, Das SM, Pultz NJ, Bonomo RA, Rice LB. Use of denaturing gradient gel electrophoresis for analysis of the stool microbiota of hospitalized patients. J Microbiol Methods. 2003;54:249–256. [PubMed]36.
Asano Y, Hiramoto T, Nishino R, et al. Critical role of gut microbiota in the production of biologically active, free catecholamines in the gut lumen of mice. Am J Physiol Gastrointest Liver Physiol. 2012;303:G1288–G1295. [PubMed]37.
Lyte M. The effect of stress on microbial growth. Anim Health Res Rev. 2014;15:172–174. [PubMed]38.
Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut:pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011;62:591–599. [PubMed]39.
Sandrini S, Alghofaili F, Freestone P, Yesilkaya H. Host stress hormone norepinephrine stimulates pneumococcal growth, biofilm formation and virulence gene expression. BMC Microbiol. 2014;14:180. [PMC free article] [PubMed]40.
Anderson MT, Armstrong SK. Norepinephrine mediates acquisition of transferrin-iron in Bordetella bronchiseptica. J Bacteriol. 2008;190:3940–3947. [PMC free article] [PubMed]41.
Glattard E, Welters ID, Lavaux T, et al. Endogenous morphine levels are increased in sepsis: a partial implication of neutrophils. PLoS One. 2010;5:e8791. [PMC free article] [PubMed]42.
Ma J, Wang J, Wan J, et al. Morphine disrupts interleukin-23 (IL-23)/IL-17-mediated pulmonary mucosal host defense against Streptococcus pneumoniae infection. Infect Immun. 2010;78:830–837. [PMC free article] [PubMed]43.
Babrowski T, Holbrook C, Moss J, et al. Pseudomonas aeruginosa virulence expression is directly activated by morphine and is capable of causing lethal gut-derived sepsis in mice during chronic morphine administration. Ann Surg. 2012;255:386–393. [PMC free article] [PubMed]44.
Banerjee S, Sindberg G, Wang F, et al. Opioid-induced gut microbial disruption and bile dysregulation leads to gut barrier compromise and sustained systemic inflammation. Mucosal Immunol. 2016;9:1418–1428. [PMC free article] [PubMed]45.
Demehri FR, Barrett M, Teitelbaum DH. Changes to the intestinal microbiome with parenteral nutrition: review of a murine model and potential clinical implications. Nutr Clin Pract. 2015;30:798–806. [PubMed]46.
Mountzouris KC, Kotzampassi K, Tsirtsikos P, Kapoutzis K, Fegeros K. Effects of Lactobacillus acidophilus on gut microflora metabolic biomarkers in fed and fasted rats. Clin Nutr. 2009;28:318–324. [PubMed]47.
Swank GM, Deitch EA. Role of the gut in multiple organ failure: bacterial translocation and permeability changes. World J Surg. 1996;20:411–417. [PubMed]48.
Shimizu K, Ogura H, Tomono K, et al. Patterns of Gram-stained fecal flora as a quick diagnostic marker in patients with severe SIRS. Dig Dis Sci. 2011;56:1782–1788. [PMC free article] [PubMed]49.
Liu Z, Qin H, Yang Z, et al. Randomised clinical trial: the effects of perioperative probiotic treatment on barrier function and post-operative infectious complications in colorectal cancer surgery - a double-blind study. Aliment Pharmacol Ther. 2011;33:50–63. [PubMed]50.
Komatsu S, Sakamoto E, Norimizu S, et al. Efficacy of perioperative synbiotics treatment for the prevention of surgical site infection after laparoscopic colorectal surgery: a randomized controlled trial. Surg Today. 2016;46:479–490. [PubMed]51.
Levesque CL, Turner J, Li J, et al. In a neonatal piglet model of intestinal failure, administration of antibiotics and lack of enteral nutrition have a greater impact on intestinal microflora than surgical resection alone. JPEN J Parenter Enteral Nutr. 2016 Feb 2; pii:0148607115626903. [Epub ahead of print] [PubMed]52.
Ralls MW, Miyasaka E, Teitelbaum DH. Intestinal microbial diversity and perioperative complications. JPEN J Parenter Enteral Nutr. 2014;38:392–399. [PMC free article] [PubMed]53.
Schardey HM, Kamps T, Rau HG, Gatermann S, Baretton G, Schildberg FW. Bacteria: a major pathogenic factor for anastomotic insufficiency. Antimicrob Agents Chemother. 1994;38:2564–2567. [PMC free article] [PubMed]54.
Olivas AD, Shogan BD, Valuckaite V, et al. Intestinal tissues induce an SNP mutation in Pseudomonas aeruginosa that enhances its virulence: possible role in anastomotic leak. PLoS One. 2012;7:e44326. [PMC free article] [PubMed]55.
Kazmierczak BI, Mostov K, Engel JN. Interaction of bacterial pathogens with polarized epithelium. Annu Rev Microbiol. 2001;55:407–435. [PubMed]56.
Engel J, Eran Y. Subversion of mucosal barrier polarity by Pseudomonas aeruginosa. Front Microbio. 2011;2:114. [PMC free article] [PubMed]57.
Engel J, Balachandran P. Role of Pseudomonas aeruginosa type III effectors in disease. Curr Opin Microbiol. 2009;12:61–66. [PubMed]58.
Shogan BD, Smith DP, Christley S, Gilbert JA, Zaborina O, Alverdy JC. Intestinal anastomotic injury alters spatially defined microbiome composition and function. Microbiome. 2014;2:35. [PMC free article] [PubMed]59.
Mack DR, Ahrne S, Hyde L, Wei S, Hollingsworth MA. Extracellular MUC3 mucin secretion follows adherence of Lactobacillus strains to intestinal epithelial cells in vitro. Gut. 2003;52:827–833. [PMC free article] [PubMed]60.
Okada M, Bothin C, Kanazawa K, Midtvedt T. Experimental study of the influence of intestinal flora on the healing of intestinal anastomoses. Br J Surg. 1999;86:961–965. [PubMed]61.
Shogan BD, Belogortseva N, Luong PM, et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci Transl Med. 2015;7:286ra68. [PMC free article] [PubMed]62.
van Praagh JB, de Goffau MC, Bakker IS, Harmsen HJ, Olinga P, Havenga K. Intestinal microbiota and anastomotic leakage of stapled colorectal anastomoses: a pilot study. Surg Endosc. 2016;30:2259–2265. [PMC free article] [PubMed]63.
Kotzampassi K, Stavrou G, Damoraki G, et al. A four-probiotics regimen reduces postoperative complications after colorectal surgery: a randomized, double-blind, placebo-controlled study. World J Surg. 2015;39:2776–2783. [PubMed]64.
Zhang JW, Du P, Gao J, Yang BR, Fang WJ, Ying CM. Preoperative probiotics decrease postoperative infectious complications of colorectal cancer. Am J Med Sci. 2012;343:199–205. [PubMed]65. Kotzampassi K, Eleftheriadis E Synbiotics in trauma: of proven benefit or a new fad. Intensive Care Units:Stress, Procedures and Mortality Rates. Nova Science Publishers; 2011. pp. 149–158.
66.
Stavrou G, Giamarellos-Bourboulis EJ, Kotzampassi K. The role of probiotics in the prevention of severe infections following abdominal surgery. Int J Antimicrob Agents. 2015;46(Suppl 1):S2–S4. [PubMed]67.
Mangell P, Thorlacius H, Syk I, et al. Lactobacillus plantarum 299v does not reduce enteric bacteria or bacterial translocation in patients undergoing colon resection. Dig Dis Sci. 2012;57:1915–1924. [PubMed]68.
He D, Wang HY, Feng JY, Zhang MM, Zhou Y, Wu XT. Use of pro-/synbiotics as prophylaxis in patients undergoing colorectal resection for cancer: a meta-analysis of randomized controlled trials. Clin Res Hepatol Gastroenterol. 2013;37:406–415. [PubMed]69.
Morrow LE, Kollef MH, Casale TB. Probiotic prophylaxis of ventilator-associated pneumonia: a blinded, randomized, controlled trial. Am J Respir Crit Care Med. 2010;182:1058–1064. [PMC free article] [PubMed]70.
Liu KX, Zhu YG, Zhang J, et al. ‘Probiotics’ effects on the incidence of nosocomial pneumonia in critically ill patients: a systematic review and meta-analysis. Crit Care. 2012;16:R109. [PMC free article] [PubMed]71.
Bo L, Li J, Tao T, et al. Probiotics for preventing ventilator-associated pneumonia. Cochrane Database Syst Rev. 2014;10:CD009066. [PMC free article] [PubMed]72.
Siempos II, Ntaidou TK, Falagas ME. Impact of the administration of probiotics on the incidence of ventilator-associated pneumonia: a meta-analysis of randomized controlled trials. Crit Care Med. 2010;38:954–962. [PubMed]73.
Barraud D, Bollaert PE, Gibot S. Impact of the administration of probiotics on mortality in critically ill adult patients: a meta-analysis of randomized controlled trials. Chest. 2013;143:646–655. [PubMed]74.
Wang J, Liu KX, Ariani F, Tao LL, Zhang J, Qu JM. Probiotics for preventing ventilator-associated pneumonia: a systematic review and meta-analysis of high-quality randomized controlled trials. PLoS One. 2013;8:e83934. [PMC free article] [PubMed]75.
Giamarellos-Bourboulis EJ, Bengmark S, Kanellakopoulou K, Kotzampassi K. Pro- and synbiotics to control inflammation and infection in patients with multiple injuries. J Trauma. 2009;67:815–821. [PubMed]76.
Koutelidakis IM, Bezirtzoglou E, Giamarellos-Bourboulis EJ, Grosomanidis V, Kotzampassi K. Impact of synbiotics on the intestinal flora of critically ill patients with multiple injuries. Int J Antimicrob Agents. 2010;36:90–91. [PubMed]77.
Kotzampassi K, Giamarellos-Bourboulis EJ, Voudouris A, Kazamias P, Eleftheriadis E. Benefits of a synbiotic formula (Synbiotic 2000 Forte) in critically Ill trauma patients: early results of a randomized controlled trial. World J Surg. 2006;30:1848–1855. [PubMed]78.
Liu ZH, Huang MJ, Zhang XW, et al. The effects of perioperative probiotic treatment on serum zonulin concentration and subsequent postoperative infectious complications after colorectal cancer surgery: a double-center and double-blind randomized clinical trial. Am J Clin Nutr. 2013;97:117–126. [PubMed]79.
Kinross JM, Markar S, Karthikesalingam A, et al. A meta-analysis of probiotic and synbiotic use in elective surgery: does nutrition modulation of the gut microbiome improve clinical outcome? JPEN J Parenter Enteral Nutr. 2013;37:243–253. [PubMed]80.
Arumugam S, Lau CS, Chamberlain RS. Probiotics and synbiotics decrease postoperative sepsis in elective gastrointestinal surgical patients: a meta-analysis. J Gastrointest Surg. 2016;20:1123–1131. [PubMed]81.
Lytvyn L, Quach K, Banfield L, Johnston BC, Mertz D. Probiotics and synbiotics for the prevention of postoperative infections following abdominal surgery: a systematic review and meta-analysis of randomized controlled trials. J Hosp Infect. 2016;92:130–139. [PubMed]82.
Tappenden KA. Probiotics are not a one-species-fits-all proposition. JPEN J Parenter Enteral Nutr. 2012;36:496. [PubMed]
Articles from Annals of Gastroenterology are provided here courtesy of The Hellenic Society of Gastroenterology
Referentielijst behorend bij Probiotics Reduce Postoperative Infections in Patients Undergoing Colorectal Surgery: A Systematic Review and Meta-Analysis
References
1.
Itatsu K., Sugawara G., Kaneoka Y., et al. Risk factors for incisional surgical site infections in elective surgery for colorectal cancer: focus on intraoperative meticulous wound management. Surgery Today. 2014;44(7):1242–1252. doi: 10.1007/s00595-013-0677-3. [PubMed] [Cross Ref]2.
Smith R. L., Bohl J. K., McElearney S. T., et al. Wound infection after elective colorectal resection. Annals of Surgery. 2004;239(5):599–605. doi: 10.1097/01.sla.0000124292.21605.99. [PMC free article] [PubMed] [Cross Ref]3.
Reddy B. S., Gatt M., Sowdi R., MacFie J. Surgical manipulation of the large intestine increases bacterial translocation in patients undergoing elective colorectal surgery. Colorectal Disease. 2006;8(7):596–600. doi: 10.1111/j.1463-1318.2006.01024.x. [PubMed] [Cross Ref]4.
Kitazawa H., Alvarez S., Suvorov A., Melnikov V., Villena J., Sánchez B. Recent advances and future perspective in microbiota and probiotics. BioMed Research International. 2015;2015:p. 2. doi: 10.1155/2015/275631.275631 [PMC free article] [PubMed] [Cross Ref]5.
Ewaschuk J., Endersby R., Thiel D., et al. Probiotic bacteria prevent hepatic damage and maintain colonic barrier function in a mouse model of sepsis. Hepatology. 2007;46(3):841–850. doi: 10.1002/hep.21750. [PubMed] [Cross Ref]6.
Bron P. A., van Baarlen P., Kleerebezem M. Emerging molecular insights into the interaction between probiotics and the host intestinal mucosa. Nature Reviews. Microbiology. 2011;10(1):66–78. doi: 10.1038/nrmicro2690. [PubMed] [Cross Ref]7.
Zareie M., Johnson-Henry K., Jury J., et al. Probiotics prevent bacterial translocation and improve intestinal barrier function in rats following chronic psychological stress. Gut. 2006;55(11):1553–1560. doi: 10.1136/gut.2005.080739. [PMC free article] [PubMed] [Cross Ref]9.
Chou H. H., Chien W. H., Wu L. L., et al. Age-related immune clearance of hepatitis B virus infection requires the establishment of gut microbiota. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(7):2175–2180. doi: 10.1073/pnas.1424775112. [PMC free article] [PubMed] [Cross Ref]10.
Parkes G. C., Sanderson J. D., Whelan K. The mechanisms and efficacy of probiotics in the prevention of Clostridium difficile-associated diarrhea. The Lancet Infectious Diseases. 2009;9(4):237–244. doi: 10.1016/S1473-3099(09)70059-3. [PubMed] [Cross Ref]11.
Wu T., Zhang Z., Liu B., et al. Gut microbiota dysbiosis and bacterial community assembly associated with cholesterol gallstones in large-scale study. BMC Genomics. 2013;14(1):p. 669. doi: 10.1186/1471-2164-14-669. [PMC free article] [PubMed] [Cross Ref]12.
Qin N., Yang F., Li A., et al. Alterations of the human gut microbiome in liver cirrhosis. Nature. 2014;513(7516):59–64. doi: 10.1038/nature13568. [PubMed] [Cross Ref]13.
Liu J., Wu D., Ahmed A., et al. Comparison of the gut microbe profiles and numbers between patients with liver cirrhosis and healthy individuals. Current Microbiology. 2012;65(1):7–13. doi: 10.1007/s00284-012-0105-8. [PubMed] [Cross Ref]14.
Neut C., Bulois P., Desreumaux P., et al. Changes in the bacterial flora of the neoterminal ileum after ileocolonic resection for Crohn’s disease. The American Journal of Gastroenterology. 2002;97(4):939–946. doi: 10.1111/j.1572-0241.2002.05613.x. [PubMed] [Cross Ref]15.
Rayes N., Seehofer D., Hansen S., et al. Early enteral supply of lactobacillus and fiber versus selective bowel decontamination: a controlled trial in liver transplant recipients. Transplantation. 2002;74(1):123–127. doi: 10.1097/00007890-200207150-00021. [PubMed] [Cross Ref]16.
Liu Z., Li C., Huang M., et al. Positive regulatory effects of perioperative probiotic treatment on postoperative liver complications after colorectal liver metastases surgery: a double-center and double-blind randomized clinical trial. BMC Gastroenterology. 2015;15(1):p. 34. doi: 10.1186/s12876-015-0260-z. [PMC free article] [PubMed] [Cross Ref]17.
Nomura T., Tsuchiya Y., Nashimoto A., et al. Probiotics reduce infectious complications after pancreaticoduodenectomy. Hepato-Gastroenterology. 2007;54(75):661–663. [PubMed]18.
Soltan Dallal M. M., Mojarrad M., Baghbani F., Raoofian R., Mardaneh J., Salehipour Z. Effects of probiotic Lactobacillus acidophilus and Lactobacillus casei on colorectal tumor cells activity (CaCo-2) Archives of Iranian Medicine. 2015;18(3):167–172. [PubMed]19.
Baldwin C., Millette M., Oth D., Ruiz M. T., Luquet F. M., Lacroix M. Probiotic Lactobacillus acidophilus and L. casei mix sensitize colorectal tumoral cells to 5-fluorouracil-induced apoptosis. Nutrition and Cancer. 2010;62(3):371–378. doi: 10.1080/01635580903407197. [PubMed] [Cross Ref]20.
Kotzampassi K., Stavrou G., Damoraki G., et al. A four-probiotics regimen reduces postoperative complications after colorectal surgery: a randomized, double-blind, placebo-controlled study. World Journal of Surgery. 2015;39(11):2776–2783. doi: 10.1007/s00268-015-3071-z. [PubMed] [Cross Ref]21.
Liu Z. H., Huang M. J., Zhang X. W., et al. The effects of perioperative probiotic treatment on serum zonulin concentration and subsequent postoperative infectious complications after colorectal cancer surgery: a double-center and double-blind randomized clinical trial. The American Journal of Clinical Nutrition. 2013;97(1):117–126. doi: 10.3945/ajcn.112.040949. [PubMed] [Cross Ref]22.
Zhang J. W., Du P., Gao J., Yang B. R., Fang W. J., Ying C. M. Preoperative probiotics decrease postoperative infectious complications of colorectal cancer. The American Journal of the Medical Sciences. 2012;343(3):199–205. doi: 10.1097/MAJ.0b013e31823aace6. [PubMed] [Cross Ref]23.
Consoli M. L., da Silva R. S., Nicoli J. R., et al. Randomized clinical trial: impact of oral administration of Saccharomyces boulardii on gene expression of intestinal cytokines in patients undergoing colon resection. JPEN Journal of Parenteral and Enteral Nutrition. 2016;40(8):1114–1121. doi: 10.1177/0148607115584387. [PubMed] [Cross Ref]24.
Komatsu S., Sakamoto E., Norimizu S., et al. Efficacy of perioperative synbiotics treatment for the prevention of surgical site infection after laparoscopic colorectal surgery: a randomized controlled trial. Surgery Today. 2016;46(4):479–490. doi: 10.1007/s00595-015-1178-3. [PubMed] [Cross Ref]25.
Sadahiro S., Suzuki T., Tanaka A., et al. Comparison between oral antibiotics and probiotics as bowel preparation for elective colon cancer surgery to prevent infection: prospective randomized trial. Surgery. 2014;155(3):493–503. doi: 10.1016/j.surg.2013.06.002. [PubMed] [Cross Ref]26.
Horvat M., Krebs B., Potrc S., Ivanecz A., Kompan L. Preoperative synbiotic bowel conditioning for elective colorectal surgery. Wiener Klinische Wochenschrift. 2010;122(Supplement 2):26–30. doi: 10.1007/s00508-010-1347-8. [PubMed] [Cross Ref]27.
Reddy B. S., Macfie J., Gatt M., Larsen C. N., Jensen S. S., Leser T. D. Randomized clinical trial of effect of synbiotics, neomycin and mechanical bowel preparation on intestinal barrier function in patients undergoing colectomy. The British Journal of Surgery. 2007;94(5):546–554. doi: 10.1002/bjs.5705. [PubMed] [Cross Ref]28.
Higgins J. P., Altman D. G., Gøtzsche P. C., et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343, article d5928 doi: 10.1136/bmj.d5928. [PMC free article] [PubMed] [Cross Ref]29.
Jadad A. R., Moore R. A., Carroll D., et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [PubMed] [Cross Ref]30.
Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [PMC free article] [PubMed] [Cross Ref]31.
Liberati A., Altman D. G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [PubMed] [Cross Ref]32.
Liu Z., Qin H., Yang Z., et al. Randomised clinical trial: the effects of perioperative probiotic treatment on barrier function and post-operative infectious complications in colorectal cancer surgery-a double-blind study. Alimentary Pharmacology & Therapeutics. 2011;33(1):50–63. doi: 10.1111/j.1365-2036.2010.04492.x. [PubMed] [Cross Ref]33.
Liu Q., Duan Z. P., Ha D. K., Bengmark S., Kurtovic J., Riordan S. M. Synbiotic modulation of gut flora: effect on minimal hepatic encephalopathy in patients with cirrhosis. Hepatology. 2004;39(5):1441–1449. doi: 10.1002/hep.20194. [PubMed] [Cross Ref]34.
D'Souza A. L., Rajkumar C., Cooke J., Bulpitt C. J. Probiotics in prevention of antibiotic associated diarrhoea: meta-analysis. BMJ. 2002;324(7350):p. 1361. [PMC free article] [PubMed]35.
Sugawara G., Nagino M., Nishio H., et al. Perioperative synbiotic treatment to prevent postoperative infectious complications in biliary cancer surgery: a randomized controlled trial. Annals of Surgery. 2006;244(5):706–714. doi: 10.1097/01.sla.0000219039.20924.88. [PMC free article] [PubMed] [Cross Ref]36.
Wildt S., Nordgaard I., Hansen U. A., Brockmann E., Rumessen J. J. Randomised double-blind placebo-controlled trial with Lactobacillus acidophilus La-5 and Bifidobacterium animalis subsp. lactis BB-12 for maintenance of remission in ulcerative colitis. Journal of Crohn's & Colitis. 2011;5(2):115–121. doi: 10.1016/j.crohns.2010.11.004. [PubMed] [Cross Ref]37.
Doherty G. A., Bennett G. C., Cheifetz A. S., Moss A. C. Meta-analysis: targeting the intestinal microbiota in prophylaxis for post-operative Crohn’s disease. Alimentary Pharmacology & Therapeutics. 2010;31(8):802–809. doi: 10.1111/j.1365-2036.2010.04231.x. [PubMed] [Cross Ref]38.
Gou S., Yang Z., Liu T., Wu H., Wang C. Use of probiotics in the treatment of severe acute pancreatitis: a systematic review and meta-analysis of randomized controlled trials. Critical Care. 2014;18(2):p. R57. doi: 10.1186/cc13809. [PMC free article] [PubMed] [Cross Ref]39.
Jeppsson B., Mangell P., Thorlacius H. Use of probiotics as prophylaxis for postoperative infections. Nutrients. 2011;3(5):604–612. doi: 10.3390/nu3050604. [PMC free article] [PubMed] [Cross Ref]40.
He D., Wang H. Y., Feng J. Y., Zhang M. M., Zhou Y., Wu X. T. Use of pro-/synbiotics as prophylaxis in patients undergoing colorectal resection for cancer: a meta-analysis of randomized controlled trials. Clinics and Research in Hepatology and Gastroenterology. 2013;37(4):406–415. doi: 10.1016/j.clinre.2012.10.007. [PubMed] [Cross Ref]41.
Machairas N., Pistiki A., Droggiti D. I., et al. Pre-treatment with probiotics prolongs survival after experimental infection by multidrug-resistant Pseudomonas aeruginosa in rodents: an effect on sepsis-induced immunosuppression. International Journal of Antimicrobial Agents. 2015;45(4):376–384. doi: 10.1016/j.ijantimicag.2014.11.013. [PubMed] [Cross Ref]42.
Borchers A. T., Selmi C., Meyers F. J., Keen C. L., Gershwin M. E. Probiotics and immunity. Journal of Gastroenterology. 2009;44(1):26–46. doi: 10.1007/s00535-008-2296-0. [PubMed] [Cross Ref]43.
Whelan K., Myers C. E. Safety of probiotics in patients receiving nutritional support: a systematic review of case reports, randomized controlled trials, and nonrandomized trials. The American Journal of Clinical Nutrition. 2010;91(3):687–703. doi: 10.3945/ajcn.2009.28759. [PubMed] [Cross Ref]44.
Szajewska H., Skórka A., Ruszczyński M., Gieruszczak-Białek D. Meta-analysis: Lactobacillus GG for treating acute gastroenteritis in children—updated analysis of randomised controlled trials. Alimentary Pharmacology & Therapeutics. 2013;38(5):467–476. doi: 10.1111/apt.12403. [PubMed] [Cross Ref]45.
Lee J. Y., Chu S. H., Jeon J. Y., et al. Effects of 12 weeks of probiotic supplementation on quality of life in colorectal cancer survivors: a double-blind, randomized, placebo-controlled trial. Digestive and Liver Disease. 2014;46(12):1126–1132. doi: 10.1016/j.dld.2014.09.004. [PubMed] [Cross Ref]46.
Geier M. S., Butler R. N., Howarth G. S. Probiotics, prebiotics and synbiotics: a role in chemoprevention for colorectal cancer? Cancer Biology & Therapy. 2006;5(10):1265–1269. [PubMed]
Articles from Gastroenterology Research and Practice are provided here courtesy of Hindawi
antibiotica, probiotica, melkzuurbacterien, Clostridium difficile infectie, bijwerkingen, diarree, operatie, infecties, darmkanker, operatie, chirurgie, ziekenhuisopname duur, herstel darmfunctie
Gerelateerde artikelen
- Probiotica en prebiotica alleen of samen als synbiotica verminderen de symptomen van depressie en angst bij patiënten met een depressie vergeleken met het niet gebruiken ervan
- Microbioom van patienten met fybromyalgie stimuleren door transplantatie met darmmicrobioom van gezonde mensen vermindert pijn en verbetert kwaliteit van leven aanzienlijk
- Bijna alle patienten met gewrichtsklachten - 92 procent - wil geïntegreerde zorg waarbij reguliere en complementaire middelen worden gecombineerd
- Omgevingsfactoren spelen grote rol in samenstelling van onze darmflora - darmmicrobiota en heeft grote invloed op onze gezondheid
- Geaccrediteerde online scholing sport, bewegen en het darmmicrobioom voor artsen en therapeuten. Data 23 mei 2024 en 4 juni 2024. Deelname is gratis.
- Leefstijl heeft grote invloed op onze gezondheid omdat de darmflora - darmmicrobiota wordt aangetast. Dagelijks probiotica kan helpen darmflora te verbeteren
- Oud verpleegkundige Basten van Huizen liep een vleesetende bacterie op die hem zwaar verminkte maar met probiotica herstelde hij zo ver dat hij weer vrijwilligerswerk kan doen
- Geaccrediteerde scholing ‘Antibiotica, levensreddend maar met welke gevolgen?’ op 8 en 13 juni 2023 via webinar vanuit Winclove Amsterdam
- Mensen met chronische maag-darmaandoeningen en symptomen van depressie of angstigheid kunnen baat hebben bij probiotica
- Probiotica voorkomt en vermindert diarree veroorzaakt door antibiotica bij kinderen blijkt uit internationaal onderzoek.
- Synbiotica ingenomen 7 dagen voor operatie bij patiënten met darmkanker vermindert kans op sterfte aan infectie, geeft korter ziekenhuisverblijf en minder gebruik van antibiotica copy 1
- Microbiologische metabolieten in ziekte en gezondheid. Een artikel dat het belang uitlegt van een goede darmflora en hoe je die kunt verbeteren
- Probiotica - melkzuurbacterien verbeteren in de dagelijkse praktijk de gezondheid van mensen, de kwaliteit van leven, minder maag-darmklachten, minder diarree en verbetert de ontlasting
- Probiotica - Melkzuurbacterien hebben gunstige invloed bij leukemiepatiënten die stamceltransplantatie moeten ondergaan.
- Probiotica gebruik in de ouderenzorg vermindert gebruik van anti-biotica en geeft veel minder diarree aldus een proefproject van de RIVAS zorggroep
- Probiotica - melkzuurbacterien verbetert kwaliteit van leven van mensen die last hebben van hooikoorts
- Praktijkrichtlijn van de Voedsel- en Landbouworganisatie van de Verenigde Naties en WHO - de Wereldgezondheidsorganisatie voor gebruik van probiotica bij darmproblemen
- Antibiotica verstoort microbiota van de darmen (Darmflora). Zelfs 1 antibioticakuur kan de darmflora al ernstig verstoren. Regelmatig antibiotica kan aan darmflora veel chronische schade toebrengen
- Microbioom van de darmen speelt grote rol in de werking van het menselijke immuunsysteem. Verbeteren van het microbioom kan positief uitpakken bij verschillende vormen van kanker
- probiotica vooraf en na operatie van maagkanker vermindert lichamelijke klachten en herstelt darmflora sneller en beter in vergelijking met placebo copy 1
- Dieet - voedingspatroon dat de darmflora beinvloed zoals vezels en probiotica heeft invloed op aanslaan van immuuntherapie met anti-PD medicijnen
- Probiotica verbetert kwaliteit van leven bij patienten met Colitus Ulcerose - prikkelbare darm
- Waarvoor dient probiotica en waar kan je dat kopen?
- Probiotica - melkzuurbacterien kunnen diarree veroorzaakt door chemo en radiotherapie bij kanker in de buik of bekken voorkomen of verminderen
- Synbiotica vooraf en na operatie van darmkanker voorkomt bijna volledig post operatieve infecties in vergelijking met placebo. 1 vs 9 uit 90 patienten. copy 1
- Synbiotica pre operatief voorkomt hoog significant ernstige complicaties bij operaties in gebied van alvleesklier. 6 versus geen sterfgevallen tijdens operatie copy 1
- Probiotica - melkzuurbacterien vooraf en na operaties bij darmkanker voorkomen ernstige infecties, bevorderen sneller herstel en zorgen voor kortere ziekenhuisopname
- Probiotica - melkzuurbacterien bestrijdt succesvol Helicobacter pylori en zorgt voor veel minder bijwerkingen van anti-biotica bij bestrijding van Helicobacter pylori
- Probiotica voorkomt Clostridium difficile infectie bij ziekenhuispatienten die anti biotica krijgen met meer dan 50 procent
- probiotica voor en na operatie van darmkanker vermindert diarree met de helft, minder infecties, versnelt herstel ontlasting en maagfunctie in vergelijking met placebo
- Probiotica - melkzuurbacteriën verminderen significant optredende diarree door chemo met irinitocan bij darmkankerpatienten. Gewone diarree 60,9 vs 39,1 procent. Ernstige diarree: 17,4 vs nul procent
- Goede darmflora - darmbacterien versterken effectiviteit van chemo bij kanker door immuunstimulatie - aanmaak extra T- killercellen - in organen buiten de darmen
- Probiotica - melkzuurbacterien verminderen significant complicaties bij darmkanker operatie en zorgen voor sneller herstel en korter verblijf in ziekenhuis
- Probiotica - melkzuurbacterien vooraf aan operatie bij darmkanker voorkomen voor een groot deel de kans op infecties ten gevolge van operatie
- Probiotica, ingenomen tijdens en na de zwangerschap, beschermt zuigelingen en kinderen tegen erfelijke allergien, maar niet tegen astma
- Probiotica vermindert significant diarree als dit ook naast antibiotica gegeven wordt bij diarree veroorzaakt door de bacterie: C. Difficile
- Probiotica - melkzuurbacteriën. Onverwachte sterfgevallen tijdens studie met probiotica en alvleesklierontsteking - wrange speling van het lot - aldus Duitse prof. Rayes die inzage kreeg in onderzoeksrapport. UMC weigert elke verdere medewerking
- Probiotica vermindert significant diarree veroorzaakt door bestraling bij patiënten met baarmoederhalskanker die daarvoor bestraald werden samen met een chemokuur
- Nieuwe studies bewijzen goed effect van probiotica, melkzuurbacteriën, bij voorkomen en genezen van diarree en darmproblemen en bestrijding van de Helicobacter Pylori, de bacterie die vaak verantwoordelijk is voor ontstaan van darm-en maagkanker.
- Probiotica - melkzuurbacteriën. Probiotica voorkomt diaree veroorzaakt door bestraling bij darmkanker, aldus gerandomiseerde dubbelblinde placebo gecontroleerde fase III studie. Artikel geplaatst 31 oktober 2007.
- Dubbelblinde gerandomiseerde fase III studie bewijst grote waarde van probiotica - melkzuurbacteriën - in versterken immuunsysteem bij kleine kinderen. Artikel geplaatst februari 2004
- Probiotica - melkzuurbacteriën. Probiotica beschermt ernstig zieke patienten aan een beademingsmachine tegen ontwikkelen van longontsteking, aldus kleinschalige Zweedse studie. Artikel geplaatst 8 maart 2008.
- Melkzuurbacteriën met ingebouwd gen moeten ziekte van Crohn voorkomen en genezen aldus nieuwe proef in AMC. Artikel geplaatst 1 juni 2003
- Melkzuurbacteriën als adjuvant / aanvulling bij bestraling bij baarmoederhalskanker.
- Probiotica voorkomt diaree of controleert diarree significant beter bij diarree ontstaan door antibioticagebruik blijkt uit grote overzichtstudie.
- Gebruik van Probiotica - Melkzuurbacteriën (Lactobacillus reuteri protectis) - reduceert het ziekteverzuim door maag- en darmproblemen met 55% blijkt uit gerandomiseerde placebo gecontroleerde studie bij 262
- Probiotica - melkzuurbacteriën (Lactobacillus- en Bifidobacteria) verbeteren significant de aanpak en vernietiging van de Helicobactor Pylori en de infecties daardoor van 85% tot 90%, zelfs bij patienten die resistent waren voor antibiotica. Hier drie ge
- Probiotica - melkzuurbacteriën. Een dagelijkse portie probiotica vermindert significant de kans op leverkanker, blijkt uit een gerandomiseerde dubbelblinde studie. Artikel geplaatst 3 juni 2006.
- Probiotica - melkzuurbacterien naast epirubicine na operatie van blaaskanker geeft significant meer driejaars ziektevrije overlevingen.
- Synbiotica (probiotica - melkzuurbacteriën plus voedingsstoffen voor bacterien) geeft aanmerkelijk minder infecties na leveroperatie.19 procent in probioticagroep t.o.v. 52 procent in controlegroep aldus gerandomiseerde studie.
- Synbiotic therapie - een combinatie van twee soorten probiotica geeft aanmerkelijk positief helend effect bij het bestrijden van ziekte van Crohn, aldus enkele gerandomiseerde studies
- Probiotica melkzuurbacteriëen: een overzicht van studies en artikelen over toepassing van probiotica naast behandelingen van kanker en herstel van darmflora na belastende behandelingen




Plaats een reactie ...
Reageer op "Probiotica - melkzuurbacterien vooraf en na operaties bij darmkanker voorkomen ernstige infecties, bevorderen sneller herstel en zorgen voor kortere ziekenhuisopname"