15 februari 2015: Bron: Sci. Signal., 10 February 2015 Vol. 8, Issue 363, p. ra15 DOI: 10.1126/scisignal.2005667
Wetenschappers hebben ontdekt waarom capsaicin, stofje dat Chilipepers heet maakt, pijnstillend werkt. Capsaicin blijkt uitstekend te werken als pijnstiller van neuralgia (pijn door beschadigde zenuwen) neuropathie (zenuwpijnen vaak ook veroorzaakt door bepaalde chemo's), spierpijnen en gewrichtspijnen (reuma, atrose).
Voor leken zal het volgende artikel niet goed te begrijpen zijn, maar wat let u eens wat meer Chilipepers te eten bij uw gewone maaltijd of Capsaicinzalf te gaan gebruiken? Of bestel capsaicin - rode peper capsules?
https://www.google.nl/?gfe_rd=cr&ei=hMDhVISYK8SwOvq4gMgB&gws_rd=ssl#q=capsaicin+capsules

En voor artsen, wetenschappers en medisch geschoolden is het interessant deze studie eens te lezen: Activation of TRPV1 channels inhibits mechanosensitive Piezo channel activity by depleting membrane phosphoinositides Het abstract staat onderaan dit artikel.
Nog interessanter is het verklarende artikel in The Scientist: How Hot Peppers Can Ease Pain. Researchers uncover one way capsaicin—the spicy compound found in chili peppers—provides pain relief.
Citaat:
The initial pain-dulling sensation occurs when capsaicin activates heat-sensing transient receptor potential vanilloid 1 (TRPV1) ion channels on sensory neurons. Prolonged stimulation with the compound results in desensitization of these neurons. “This is one of the underlying mechanisms of capsaicin’s numbing effect, but TRPV1 is a heat sensor, so how it affects mechanical pain was not known,” said Tibor Rohacs, an associate professor of pharmacology and physiology at Rutgers New Jersey Medical School, who led the study.
Rohacs and his colleagues uncovered a link between the heat-stimulating function of capsaicin and its ability to relieve mechanical pain including neuralgia (pain from damaged nerves), neuropathy, and muscle and joint pain. Capsaicin’s activation of TRPV1 ion channels in turns inhibits mechanical force-sensing ion channels called Piezo1 and 2 by depleting phospholipid signaling molecules, phosphoinositides, in the cell membrane.
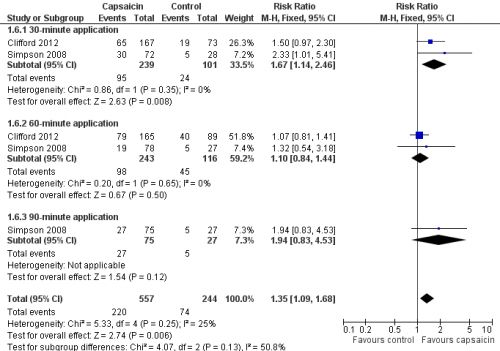
In 2013 publiceerden onderzoekers een reviewstudie naar effecten van hoge concentratie capsaicinzalf met mooie resultaten: Topical capsaicin (high concentration) for chronic neuropathic pain in adults
AUTHORS' CONCLUSIONS:
High-concentration topical capsaicin used to treat postherpetic neuralgia and HIV-neuropathy generates more participants with high levels of pain relief than does control treatment using a much lower concentration of capsaicin. The additional proportion who benefit over control is not large, but for those who do obtain high levels of pain relief there are additional improvements in sleep, fatigue, depression and an improved quality of life. High-concentration topical capsaicin is therefore similar to other therapies for chronic pain. In this case, the high cost of single and repeated applications suggest that high-concentration topical capsaicin is likely to be used when other available therapies have failed, and that it should probably not be used repeatedly without substantial documented pain relief. Even when efficacy is established, there are unknown risks, especially on epidermal innervation, of repeated application of long periods.
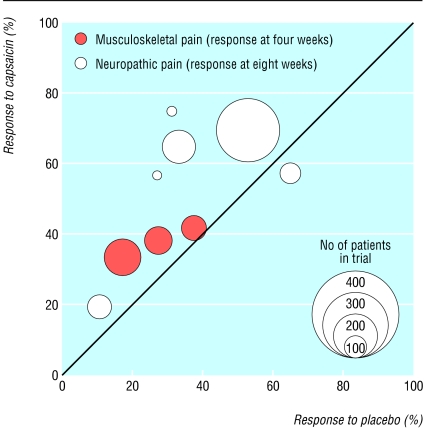
The Cochane Library publiceerde in 2004 een review van tot dan gepubliceerde placebo gecontroleerde studies naar capsaicinzalf. Dus niet naar capsaicin uit Chilipepers: Systematic review of topical capsaicin for the treatment of chronic pain
Conclusie daaruit is dat vergeleken met placebo het enig effect gaf (nog altijd 35% vermindering van de pijn tegenover 25% bij placebo) maar dat capsaicinzalf niet wordt aanbevolen. Maar als je de referentielijst bekijkt, zie onderaan artikel, dan lijkt capsaicinzalf toch wel behoorlijk goed te kunnen werken.En afgaande op recente studie lijkt het eten van Chilipepers zeker de moeite waard te proberen.
Abstracten staan onderaan artikel.
10 april 2006: Bron: J Clin Oncol. 1997 Aug;15(8):2974-80.
Capsaicin zalf, (het stofje capsaicin zit in rode pepers en maakt deze dat pepers als heet/scherp worden ervaren) voorkomt hoog significant neurologische pijn (zenuwpijnen) bij kankerpatiënten die geopereerd worden aan hun kanker. Wij vertaalden voor u het abstact van deze studie, die al in 1997 !!!!! werd gepubliceerd. Zie ook positief effect van gebruik van capsaicin zelf bij prostaatkanker: Capsaicin is een stofje dat veel voorkomt in rode pepers bevordert apoptosis = zelfdoding van prostaatkankercellen.
Fase III placebo-gecontroleerde trial van capsaicin zalf in de behandeling van operatieve neuropathische pijn (zenuwpijn) bij kankerpatiënten.
Ellison N, Loprinzi CL, Kugler J, Hatfield AK, Miser A, Sloan JA, Wender DB, Rowland KM, Molina R, Cascino TL, Vukov AM, Dhaliwal HS, Ghosh C.
Geisinger Clinical Oncology Program, Danville, PA, USA.
DOEL: Een minderheid van kanker overlevenden ontwikkelen postoperatieve (na de operatie) en op lange termijn zenuwpijn. Gebaseerd op het bewijs dat capsaicin, het scherpe/hete ingrediënt in hot chili pepers, nuttig zou kunnen zijn in het behandelen van zenuwpijn, ontwikkelden we deze klinische trial.
PATIENTEN EN METHODEN: 99 geschikte patiënten met postoperatieve zenuwpijn werden toegelaten tot deze studie. Na stratificatie (verdeling in groepen), werden de patiënten 8 weken lang capsaicin zalf gegeven (0.075% capsaicin bevattend) gevolgd door 8 weken van een indentieke placebo zalf, of omgekeerd. De capsaicin/placebo zalf werd vier keer per dag op de pijnlijke plekken gesmeerd. Evaluatie van de behandeling werd uitgevoerd door middel van wekelijkse vragenlijsten die door de patiënten werden ingevuld.
RESULTATEN: Gedurende de eerste 8-weken periode, de capsaicin-zalf toediening werd geassocieerd met substantieel meer huidverbranding, huid roodheid en hoesten (P < .0001 voor lek). Echter de behandeling met capsaicin werd net zo vaak gestopt door de weigering van de patiënt of toxiciteit dan in de placebogroep. De capsaicin zalfgroep had substantieel (statistich significant) meer pijnverlichting (P = .01) na de eerste 8 weken, met een gemiddelde pijnverlichting van 53% tegenover 17%. Na completering van de 16 weken durende studie, werd aan de patiënten gevraagd welke behandelingsperiode het meest profijtelkjik was. Van de reagerende patiënten koos 60% de capsaicin periode, 18% koos de placebo periode, en 22% koos geen enkele periode (P = .001).
CONCLUSIE: Een uitwendige capsaicin zalf vermindert postoperatieve zenuwpijn en ondanks enkele bijwerkingen werd deze capsaicin zalf drie keer zo vaak verkozen door de patiënten boven de placebozalf.
Publication Types:
Clinical Trial
Clinical Trial, Phase III
Randomized Controlled Trial
PMID: 9256142 [PubMed - indexed for MEDLINE]
J Clin Oncol. 1997 Aug;15(8):2974-80
Phase III placebo-controlled trial of capsaicin cream in the management of surgical neuropathic pain in cancer patients.
Ellison N, Loprinzi CL, Kugler J, Hatfield AK, Miser A, Sloan JA, Wender DB, Rowland KM, Molina R, Cascino TL, Vukov AM, Dhaliwal HS, Ghosh C.
Geisinger Clinical Oncology Program, Danville, PA, USA.
PURPOSE: A minority of cancer survivors develops long-term postsurgical neuropathic pain. Based on evidence that capsaicin, the pungent ingredient in hot chili peppers, might be useful for treating neuropathic pain, we developed the present clinical trial.
PATIENTS AND METHODS: Ninety-nine assessable patients with postsurgical neuropathic pain were entered onto this study. After stratification, patients were to receive 8 weeks of a 0.075% capsaicin cream followed by 8 weeks of an identical-appearing placebo cream, or vice versa. A capsaicin/placebo cream was to be applied to the painful site four times daily. Treatment evaluation was performed by patient-completed weekly questionnaires.
RESULTS: During the first 8-week study period, the capsaicin-cream arm was associated with substantially more skin burning, skin redness, and coughing (P < .0001 for each). Nonetheless, treatment was stopped for patient refusal or toxicity just as often while patients were receiving the placebo as compared with the capsaicin. The capsaicin cream arm had substantially more pain relief (P = .01) after the first 8 weeks, with an average pain reduction of 53% versus 17%. On completion of the 16-week study period, patients were asked which treatment period was most beneficial. Of the responding patients, 60% chose the capsaicin arm, 18% chose the placebo arm, and 22% chose neither (P = .001).
CONCLUSION: A topical capsaicin cream decreases postsurgical neuropathic pain and, despite some toxicities, is preferred by patients over a placebo by a three-to-one margin among those expressing a preference.
Publication Types:
Clinical Trial
Clinical Trial, Phase III
Randomized Controlled Trial
PMID: 9256142 [PubMed - indexed for MEDLINE]
How Hot Peppers Can Ease Pain Researchers uncover one way capsaicin—the spicy compound found in chili peppers—provides pain relief.
Activation of TRPV1 channels inhibits mechanosensitive Piezo channel activity by depleting membrane phosphoinositides
- Istvan Borbiro,
- Doreen Badheka, and
- Tibor Rohacs*
- Author Affiliations
- Department of Pharmacology and Physiology, Rutgers New Jersey Medical School, Newark, NJ 07103, USA.
- *Corresponding author. E-mail: tibor.rohacs@rutgers.edu
Abstract
Capsaicin is an activator of the heat-sensitive TRPV1 (transient receptor potential vanilloid 1) ion channels and has been used as a local analgesic. We found that activation of TRPV1 channels with capsaicin either in dorsal root ganglion neurons or in a heterologous expression system inhibited the mechanosensitive Piezo1 and Piezo2 channels by depleting phosphatidylinositol 4,5-bisphosphate [PI(4,5)P2] and its precursor phosphatidylinositol 4-phosphate [PI(4)P] from the plasma membrane through Ca2+-induced phospholipase Cδ (PLCδ) activation. Experiments with chemically inducible phosphoinositide phosphatases and receptor-induced activation of PLCβ indicated that inhibition of Piezo channels required depletion of both PI(4)P and PI(4,5)P2. The mechanically activated current amplitudes decreased substantially in the excised inside-out configuration, where the membrane patch containing Piezo1 channels is removed from the cell. PI(4,5)P2 and PI(4)P applied to these excised patches inhibited this decrease. Thus, we concluded that Piezo channel activity requires the presence of phosphoinositides, and the combined depletion of PI(4,5)P2 and PI(4)P reduces channel activity. In addition to revealing a role for distinct membrane lipids in mechanosensitive ion channel regulation, these data suggest that inhibition of Piezo2 channels may contribute to the analgesic effect of capsaicin.
Citation:
I. Borbiro, D. Badheka, and T. Rohacs, Activation of TRPV1 channels inhibits mechanosensitive Piezo channel activity by depleting membrane phosphoinositides. Sci. Signal. 8, ra15 (2015).Although topically applied capsaicin has moderate to poor efficacy in the treatment of chronic musculoskeletal or neuropathic pain, it may be useful as an adjunct or sole therapy for a small number of patients who are unresponsive to, or intolerant of, other treatments.
Systematic review of topical capsaicin for the treatment of chronic pain
References for topical capsaicin in painrelief
1. Nolano M, Simone DA, Wendelschafer-Crabb G, Johnson T, Hazen E, Kennedy WR. Topical capsaicin in humans: parallel loss of epidermal nerve fibres and pain sensation. Pain 1999;81: 135-45.
2. Reynolds JEF ed. Martindale: the extra pharmacopoeia. 32nd edn. London: Royal Pharmaceutical Society, 1999.
3. British Medical Association. Royal Pharmaceutical Society of Great Britain. British national formulary. London: BMA, RPS, 2003. (No 45.)
4. Prescription cost analysis. England 2002. Department of Health, London. 2003 ISBN 1 84182 710 X. www.doh.gov.uk/prescriptionstatistics/index.htm
5. Rains C, Bryson HM. Topical capsaicin. A review of its pharmacological properties and therapeutic potential in post-herpetic neuralgia, diabetic neuropathy and osteoarthritis. Drugs Aging 1995;7: 317-28.
6. Jadad AR, Carroll D, Moore A, McQuay H. Developing a database of published reports of randomised clinical trials in pain research. Pain 1996;66: 239-46.
7. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17: 1-12.
8. Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain 2000;86: 119-32.
9. Moore RA, Tramer MR, Carroll D, Wiffen PJ, McQuay HJ. Quantitative systematic review of topically applied non-steroidal anti-inflammatory drugs. BMJ 1998;316: 333-8. [PMC free article]
10. Cook D, Sackett DL. On the clinically important difference. Ann Intern Med 1992;117: A16-7.
11. Morris JA, Gardner MJ. Calculating confidence intervals for relative risk, odds ratios and standardised ratios and rates. In: Gardner MJ, Altman DG, eds. Statistics with confidence—confidence intervals and statistical guidelines. London: British Medical Journal, 1995: 50-63.
12. Tramer MR, Reynolds DJ, Moore RA, McQuay HJ. Impact of covert duplicate publication on meta-analysis: a case study. BMJ 1997;315: 635-40. [PMC free article]
13. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 1999;354: 1896-900.
14. L'Abbe KA, Detsky AS, O'Rourke K. Meta-analysis in clinical research. Ann Intern Med 1987;107: 224-33.
15. Zhang WY, Li Wan Po A. The effectiveness of topically applied capsaicin. A meta-analysis. Eur J Clin Pharmacol 1994;46: 517-22.
16. The Capsaicin Study Group. Treatment of painful diabetic neuropathy with topical capsaicin. A multicenter, double-blind, vehicle-controlled study. Arch Intern Med 1991;151: 2225-9.
17. Chad DA, Aronin N, Lundstrom R, McKeon P, Ross D, Molitch M, et al. Does capsaicin relieve the pain of diabetic neuropathy? Pain 1990;42: 387-8.
18. Deal CL, Schnitzer TJ, Lipstein E, Seibold JR, Stevens RM, Levy MD, et al. Treatment of arthritis with topical capsaicin: a double-blind trial. Clin Ther 1991;13: 383-95.
19. Bernstein JE, Korman NJ, Bickers DR, Dahl MV, Millikan LE. Topical capsaicin treatment of chronic postherpetic neuralgia. J Am Acad Dermatol 1989;21: 265-70.
20. Watson CP, Evans RJ. The postmastectomy pain syndrome and topical capsaicin: a randomized trial. Pain 1992;51: 375-9.
21. Altman RD, Aven A, Holmburg CE, Pfeifer LM, Sack M, Young GT. Capsaicin cream 0.025% as monotherapy for osteoarthritis: a double-blind study. Semin Arthritis Rheum 1994;23: 25-33.
22. Keitel W, Frerick H, Kuhn U, Schmidt U, Kuhlmann M, Bredehorst A. Capsicum pain plaster in chronic non-specific low back pain. Arzneimittelforschung 2001;51: 896-903.
23. Ellison N, Loprinzi CL, Kugler J, Hatfield AK, Miser A, Sloan JA, et al. Phase III placebo-controlled trial of capsaicin cream in the management of surgical neuropathic pain in cancer patients. J Clin Oncol 1997;15: 2974-80.
24. Low PA, Opfer-Gehrking TL, Dyck PJ, Litchy WJ, O'Brien PC. Double-blind, placebo-controlled study of the application of capsaicin cream in chronic distal painful polyneuropathy. Pain 1995;62: 163-8.
25. Watson CP, Tyler KL, Bickers DR, Millikan LE, Smith S, Coleman E. A randomized vehicle-controlled trial of topical capsaicin in the treatment of postherpetic neuralgia. Clin Ther 1993;15: 510-26.
26. Biesbroeck R, Bril V, Hollander P, Kabadi U, Schwartz S, Singh SP, et al. A double-blind comparison of topical capsaicin and oral amitriptyline in painful diabetic neuropathy. Adv Ther 1995;12: 111-20.
27. Schnitzer TJ, Posner M, Lawrence ID. High strength capsaicin cream for osteoarthritis pain: rapid onset of action and improved efficacy with twice daily dosing. J Clin Rheumatol 1995;1: 268-73.
28. Schnitzer T, Morton C, Coker S. Topical capsaicin therapy for osteoarthritis pain: achieving a maintenance regimen. Semin Arthritis Rheum 1994;23: 34-40.
29. Winocur E, Gavish A, Halachmi M, Eli I, Gazit E. Topical application of capsaicin for the treatment of localized pain in the temporomandibular joint area. J Orofac Pain 2000;14: 31-6.
30. McCleane G. Topical application of doxepin hydrochloride, capsaicin and a combination of both produces analgesia in chronic human neuropathic pain: a randomized, double-blind, placebo-controlled study. Br J Clin Pharmacol 2000;49: 574-9. [PMC free article]
31. Paice JA, Ferrans CE, Lashley FR, Shott S, Vizgirda V, Pitrak D. Topical capsaicin in the management of HIV-associated peripheral neuropathy. J Pain Symptom Manage 2000;19: 45-52.
32. Naylor CD, Chen E, Strauss B. Measured enthusiasm: does the method of reporting trial results alter perceptions of therapeutic effectiveness? Ann Intern Med 1992;117: 916-21.
33. Moore R, Edwards J, Barden J, McQuay H. Bandolier's little book of pain. Oxford: Oxford University Press, 2003: 238-40.
34. Kalso E, Moore RA. Five easy pieces on evidence-based medicine (2). Eur J Pain 2000;4: 321-4.
35. Song F, Altman DG, Glenny AM, Deeks JJ. Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published meta-analyses. BMJ 2003;326: 472. [PMC free article]
36. Mason L, Moore RA, Edwards JE, McQuay HJ, Wiffen PJ. Systematic review of efficacy of topical rubefacients containing salicylates for the treatment of acute and chronic pain. BMJ; 2004:doi:10.1136/bmj.38040.607141. [PMC free article]
37. Moore RA, Gavaghan D, Tramer MR, Collins SL, McQuay HJ. Size is everything—large amounts of information are needed to overcome random effects in estimating direction and magnitude of treatment effects. Pain 1998;78: 209-16.
38. Gøtzsche PC. Reporting of outcomes in arthritis trials measured on ordinal and interval scales is inadequate in relation to meta-analysis. Ann Rheum Dis 2001;60: 349-52. [PMC free article]
39. Simone DA, Nolano M, Johnson T, Wendelschafer-Crabb G, Kennedy WR. Intradermal injection of capsaicin in humans produces degeneration and subsequent reinnervation of epidermal nerve fibres: correlation with sensory function. J Neurosci 1998;18: 8947-59.
High-concentration topical capsaicin used to treat postherpetic neuralgia and HIV-neuropathy generates more participants with high levels of pain relief than does control treatment using a much lower concentration of capsaicin.
Topical capsaicin (high concentration) for chronic neuropathic pain in adults.
Abstract
BACKGROUND:
Topical creams with capsaicin are used to treat peripheral neuropathic pain. Following application to the skin capsaicin causes enhanced sensitivity, followed by a period with reduced sensitivity and, after repeated applications, persistent desensitisation. High-concentration (8%) capsaicin patches were developed to increase the amount of capsaicin delivered; rapid delivery was thought to improve tolerability because cutaneous nociceptors are 'defunctionalised' quickly. The single application avoids noncompliance. Only the 8% patch formulation of capsaicin is available, with a capsaicin concentration about 100 times greater than conventional creams.High-concentration topical capsaicin is given as a single patch application to the affected part. It must be applied under highly controlled conditions, normally under local anaesthetic, due to the initial intense burning sensation it causes. The benefits are expected to last for about 12 weeks, when another application might be made.
OBJECTIVES:
To review the evidence from controlled trials on the efficacy and tolerability of topically applied, high-concentration (8%) capsaicin in chronic neuropathic pain in adults.
SEARCH METHODS:
We searched CENTRAL, MEDLINE, EMBASE and clinicaltrials.gov to December 2012.
SELECTION CRITERIA:
Randomised, double-blind, placebo-controlled studies of at least six weeks' duration, using topical capsaicin to treat neuropathic pain.
DATA COLLECTION AND ANALYSIS:
Two review authors independently assessed trial quality and validity, and extracted data on numbers of participants with pain relief (clinical improvement) after at least six weeks, and with local skin reactions. We calculated risk ratio and numbers needed to treat to benefit (NNT) and harm (NNH). We sought details of definition of pain relief and specific adverse events.Efficacy outcomes reflecting long-duration pain relief after a single drug application were from the patient global impression of change (PGIC) at specific points, usually eight and 12 weeks. We regarded these outcomes as first-tier evidence. We regarded average pain scores over weeks 2 to 8 and 2 to 12 and the number and/or percentage of participants with pain intensity reduction of at least 30% or at least 50% over baseline as second-tier evidence.
MAIN RESULTS:
We included six studies, involving 2073 participants; they were of generally good reporting quality; the control was 0.04% topical capsaicin to help maintain blinding. Efficacy outcomes were inconsistently reported between studies, however, resulting in analyses for most outcomes being based on less than complete data.Four studies involved 1272 participants with postherpetic neuralgia. All efficacy outcomes were significantly better than control. At both eight and 12 weeks there was a significant benefit for high-concentration over low-concentration topical capsaicin for participants reporting themselves to be much or very much better, with point estimates of the NNTs of 8.8 (95% confidence interval (CI) 5.3 to 26) and 7.0 (95% CI 4.6 to 15) respectively. More participants had average 2 to 8-week and 2 to 12-week pain intensity reductions over baseline of at least 30% and at least 50% with active treatment than control, with NNT values between 10 and 12.Two studies involved 801 participants with painful HIV-neuropathy. In a single study the NNT at 12 weeks for participants to be much or very much better was 5.8 (95% CI 3.8 to 12). Over both studies more participants had average 2 to 12-week pain intensity reductions over baseline of at least 30% with active treatment than control, with an NNT of 11.Local adverse events were common, but not consistently reported. Serious adverse events were no more common with active treatment (4.1%) than control (3.2%). Adverse event withdrawals did not differ between groups, but lack of efficacy withdrawals were somewhat more common with control than active treatment, based on small numbers of events. No deaths were judged to be related to study medication.
AUTHORS' CONCLUSIONS:
High-concentration topical capsaicin used to treat postherpetic neuralgia and HIV-neuropathy generates more participants with high levels of pain relief than does control treatment using a much lower concentration of capsaicin. The additional proportion who benefit over control is not large, but for those who do obtain high levels of pain relief there are additional improvements in sleep, fatigue, depression and an improved quality of life. High-concentration topical capsaicin is therefore similar to other therapies for chronic pain. In this case, the high cost of single and repeated applications suggest that high-concentration topical capsaicin is likely to be used when other available therapies have failed, and that it should probably not be used repeatedly without substantial documented pain relief. Even when efficacy is established, there are unknown risks, especially on epidermal innervation, of repeated application of long periods.
Update of
- Topical capsaicin for chronic neuropathic pain in adults. [Cochrane Database Syst Rev. 2009]
- PMID:
- 23450576
- [PubMed - indexed for MEDLINE]
Gerelateerde artikelen
- Alternatieve therapieën bij kanker: een waarschuwing vooraf
- Algemene artikelen over complementaire bewezen middelen en behandelingen
- Ayurvedische kruiden en middelen aanvullend op chemo verminderen sterk de bijwerkingen zoals vermoeidheid, overgeven en misselijkheid veroorzaakt door chemotherapie bij kankerpatiënten met verschillende vormen van kanker, ongeacht stadium, orgaan enz.
- Voorlichtingsfilmpjes over complementaire behandelingen en middelen waaronder voedingsuppletie als preventie en aanvullende behandeling bij kanker.
- Agaricus Blazei Murill een paddestoel met medicinale kwaliteiten
- Aids - HIV en effect van voeding en voedingstoffen: 60 mg. retinol ( 200.000 IE) - vitamine A per dag gegeven aan kinderen besmet met het HIV virus geeft 40 procent minder sterfte gerekend over periodes van drie maanden.
- Aldara zalf - Imiquimod, een zalf voornamelijk gebruikt bij vormen van niet melanome huidkanker en andere huid aandoeningen zoals genitale wratten.
- Aloe Vera naast chemo bij solide tumoren geeft significant beter effect in verkleinen tumoren en geeft mediaan langere levensduur. Blijkt uit gerandomiseerde fase III studie. Artikel geplaatst 9 maart 2010
- AMAS test - Anti Maligne Antibody Serum test - geeft 95% zekerheid voor vaststellen van vroege primaire borstkanker en 99% voor vaststellen van recidief van borstkanker, maar de AMAS test geldt ook voor andere vormen van kanker als betrouwbare diagnose.
- Antioxidanten, voeding en vitamines en mineralen als preventie en medicijn tegen kanker: een aantal belangrijke studies en artikelen bij elkaar gezet
- Antineoplaston therapie van dr. Burzynski .Laatst bekende resultaten van trials met Burzinky's antineoplastontherapie bij vooral hersentumoren maar ook bij o.a. darmkanker en andere kankersoorten
- Apatone, een combinatie van vitamine C en vitamine K3, geeft goede resultaten bij prostaatkanker, endometriosekanker, eierstokkanker en andere vormen van kanker via autoschizis, geactiveerde celdood
- Artemisinin, een aantal artikelen bij elkaar gezet. Zie ook onder Chinese kruiden bij complemenatair voor veel meer informatie over TCM - traditionele Chinese kruiden bij vele vormen van kanker
- Arabinoxylaan wat is het en wat kan het betekenen als aanvullend middel bij kanker?
- Artemisinin: Artemesia of ook wel Artimisinin, een Chinees kruid, lijkt van grote waarde in een behandeling van kanker. Vooral bij hormoongevoelige kankersoorten.
- Ascorbinezuur.: Effect van intraveneuze toediening van ascorbinezuur (intraveneuze injecties met vitamine C) als aanvulling in kankerbehandeling lijkt veelbelovend
- Belladonna, een homeopatisch middel, bevordert in gerandomiseerd, dubbelblind onderzoek herstel van bijwerkingen van bestraling.
- Bestraling en effecten van voeding en voedingstoffen daarbij.. Hier een aantal studies en artikelen bij elkaar gezet over dit onderwerp.
- Betaglucaan (Bèta 1.3 Glucaan), een stofje uit medicinale paddestoelen en waarom dit natuurlijke middel zo bijzonder is in een behandeling van kanker. Lees hier naast informatie wat Betaglucaan is ook enkele studies over en met Betaglucaan.
- Bewegen en sporten voorkomt en herstelt ernstige vermoeidheid bij kankerpatienten blijkt uit grote studies. Iedere kankerpatient zou een bewegingsprogramma moeten worden voorgeschreven aldus de onderzoekers.
- Boeken over aanvullende en alternatieve behandelingswijzen en natuurlijke middelen: Bv. Het grootste en eerlijkste anti-hormonenboek: Femmes si vous saviez: Wat alle vrouwen zouden moeten weten over vooral de rol van hormonen in relatie tot baarmoederhals
- Bosbessen uit Australie (EBC-46) genezen kanker bij enkele patienten binnen enkele weken wanneer ingespoten direct in de tumor.
- Champignons bewerkt met speciale belichting hebben daarmee veel extra vitamine D en kunnen vitamine-D supplementen vervangen
- Cranberrysap en cranberrysuppletie verminderen aanzienlijk het risico op urineweginfecties bij daarvoor gevoelige mensen blijkt uit grote meta-analyse studie
- Crocine van saffraan (Crocus sativus L.) voorkomt neuropathie in vergelijking met een placebo bij kankerpatienten die chemo kregen
- Acupunctuur als aanvulling in een behandeling van kanker of behandelen van bijwerkingen veroorzaakt door bv. chemokuren bij elkaar gezet in aparte artikelenreeks
- Capsaicin zalf uitwendig aangebracht, vermindert significant neurologische pijn (zenuwpijnen) veroorzaakt door operatieve ingrepen bij kankerpatiënten maar chilipepers met veel capsaicin werken ook goed als pijnstiller.
- Chlorophyl uit o.a. spinazie compenseert kankerverwekkend effect van haem, een stofje veel en voornamelijk voorkomend in rood vlees
- citruspectine is volgens arts-bioloog drs. Engelbert Valstar een effectief voedingssupplement bij o.a. prostaatkanker en darmkanker
- Corolius Versicolor - een medicinale paddestoel zorgt al na twee maanden voor 65 tot 77% verhoogde T-cel activiteit bij 36 patiënten met het CMV = Chronisch Vermoeidheids Syndroom en/of verstoorde immuunfunctie.
- Darmkanker en niet-toxische aanvullende middelen: een overzicht van bewezen effectieve niet-toxische behandelingen, middelen en voedingstoffen
- DCA - Dichloroacetate informatie
- DHEA een uitstekend natuurlijk alternatief voor hormoontherapie bij postmenopausale vrouwen - 50 tot 65 jaar
- DMSO - Dimethyl sulfoxide blijft een middel dat effectief een rol kan spelen bij beroertes, pijnstilling, weefselletsel, auto-immuuunziektes en zelfs bij kankerpatienten zorgt voor remissies
- Echinacea-extracten bij vrouwen met voorstadium van baarmoederhalskanker en verhoogde L-SIL/CIN-1 waarden verkregen uit uitstrijkjes doet HPV infectie en voorstadium kanker sneller verdwijnen na 6 maanden en 1 jaar.
- Ellagic acid, een natuurlijk middel in een behandeling of preventie van kanker
- EPO zorgt onverwacht voor negatief effect op overleving bij hoofd- halstumoren, aldus gerandomiseerde fase III studie.
- Endometriosekanker: Voedingstoffen zoals voedingsvezels, aanvullende vitamines en dan specifiek vitamines C, E en Betacaroteen en Retinol kunnen het risico op endometriosekanker aanmerkelijk verlagen.
- Enzymtherapie van dr. Gonzalez, een overzicht met alle publicaties en studies
- EPA - eicosapentaenoic acid (een Omega-3 vetzuur) naast chemo zorgt significant voor meer remissies bij kinderen met leukemie en zij hebben significant minder gewichtsverlies aldus gerandomiseerde fase II studie.
- Essiac en Flor-Essence informatie
- Gabapentin gaat opvliegers net zo goed tegen als oestrogeen blijkt uit dubbelblind gerandomiseerde studie. Artikel geplaatst 12 juli 2006
- Genisteïne gaat opvliegers significant tegen blijkt uit dubbelblinde gerandomiseerde studie bij 90 gezonde vrouwen van 47 tot 57 jaar in de overgang gedurende 1 jaar follow-up.
- Ginseng: De waarde van Ginseng in een behandeling van kanker en tegengaan van bijwerkingen. Een overzichtsartikel voor artsen en voedingsdeskundigen. Artikel geplaatst 12 december 2009
- Glutamine tijdens chemotherapie bij darmkanker vermindert significant de kans op neuropathische problemen daarna.
- Groene thee. Wat is het en de werking ervan? Met ondersteunende literatuur.
- Haaienkraakbeen geeft geen positief effect in vergelijking met placebo bij kankerpatiënten aldus kleine maar wel gerandomiseerde studie bij totaal 83 patiënten met darmkanker en borstkanker.
- Haelan, een natuurlijk drankje gebaseerd op soja met medicinale kwaliteiten
- Huidkanker en zalven: Black Salve -Balm of Gilead , Cansemazalf, Aldarazalf, allemaal zalven op natuurlijke basis. Hier een aantal studies en publicaties over deze zalven voor huidkanker en huidaandoeningen
- Hyaluronzuur vermindert kans op bloedingen van blaas en pijn aan het bekken door bestraling net zo goed als hyperbare zuurstof maar is veel gemakkelijker toe te dienen.
- Hyperbare zuurstoftherapie voorkomt door bestraling veroorzaakte blaasontstekingen bij patienten die op het bekkengebied waren bestraald.
- Hyperthermie en effect bij verschillende kankersoorten en als aanvulling op zowel chemo kuren als bij bestraling. Vele studies bewijzen effect van hyperthermie en zijn bij elkaar gezet in aparte artikelen reeks.
- Honing als medicijn: hier een aantal artikelen over het effect van honing in het tegengaan van bijwerkingen bij chemo en bestraling bij verschillende soorten kanker
- Immuunstimulerende voedingstoffen 7 dagen voor en 5 dagen na operatie van darmkanker vermindert significant infecties en bevordert sneller herstel
- Indole-3-carbinol (I3C), een natuurlijk voedingssupplement voor gebruik bij kanker voor o.a. hormoongevoelige vormen van kanker
- Isoflavonen gaan tegenover placebo aantoonbaar botverlies tegen bij vrouwen in de overgang
- IJzer de gevaren van een noodzakelijk mineraal, door Alf Knutzen, orthomoleculair voedingsdeskundige copy 1
- Kombucha thee wat is het? hoe werkt het? Hoe maak je het?
- Koorts en kanker: Opvallend veel spontane genezingen van kanker zijn vaak veroorzaakt door infecties en koorts. Hier een artikel met voorbeelden van genezen kankerpatienten.
- Koper - negatief - en magnesium - positief - spelen een significante rol bij risico op overlijden gerelateerd ook aan hart- en vaatziektes en kanker.
- Kurkuma - curcumine heeft een sterke anti kankerwerking, een overzicht van belangrijke studies met kurkuma - curcumine
- LDN - Low Dose Naltrexone is een niet toxisch middel dat voor enkele toepassingen goedgekeurd is door de FDA
- Leefstijl: Gezond dieet met vloeibaar eten gedurende 3 tot 5 maanden en stapsgewijs onder begeleiding terug naar vast voedsel en gezonde leefstijl geneest met 48 tot 73 procent van de patienten met diabetes 2
- Lipo-ATRA - all-trans retinoic acid - vitamine A - verpakt in vetbolletjes en inwendig ingebracht zorgt voor opvallend groot aantal totale remissies bij 34 patiënten met APL - acute promyelocytic leukemia, die geen chemo hadden gehad
- Longkanker: Complementaire - aanvullende niet toxische behandelingen en middelen bij longkanker: een overzicht
- Low level laser voorkomt en geneest mucositis - aantasting van de slijmvliezen in de mond veroorzaakt door stamceltransplantatie, chemo of bestraling. Nu met Nederlands apparaatje ook zelf thuis te gebruiken.
- Lycopeen blijkt uitstekend middel in voorkomen en remmen van prostaatkanker, maar heeft ook nog andere kwaliteiten, zie hier een aantal artikelen over lycopeen
- MACA is een natuurlijk middel dat veel gebruikt wordt voor het optimaliseren van het immuunsysteem en vitaliteit en ook wel door kankerpatiënten wordt gebruikt.
- Magnesium per infuus verbetert bij de helft van de patienten met chronische migraine de pijn en ongemak met meer dan 30 procent
- Maitake MD-fraction: De medicinale paddestoel Maitake MD-fraction , waarom dit natuurlijke middel zo bijzonder is in een behandeling van kanker
- Maretakinjecties (Iscador, Abnoba) : Alle bekende en beschikbare studieresultaten over maretakinjecties bij kanker op een rijtje gezet.
- Marihuana - cannabis als medicijn en als pijnstiller en wellicht als medicijn bij Alzheimer - dementie
- Mastic gum (mastika) laat maagzweren verdwijnen en voorkomt maagzweren, maar lijkt ook goed in bestrijding van maag- en darmkanker en ziekte van Crohn.
- Mebendazole (MBZ) een antiparasieten middeltje blijkt uitstekend medicijn tegen verschillende vormen van kanker en nagenoeg zonder bijwerkingen.
- Melatonine, een overzicht van artikelen over melatonine als aanvulling bij een kankerbehandeling bij elkaar gezet.
- Menatetrenone ( = analoog aan vitamine K2) vermindert bij operabele leverkanker de kans op een recidief significant - 42,7 % na 1 jaar en 27,3% na 3 jaar ) en verbetert 3 jaars overleving met 23 %.
- Mycamine - Micafungin sodium - een stofje uit medicinale paddestoelen en een betaglucaan 1.3 krijgt van FDA erkenning als medicijn ter preventie en behandeling tegen candida infecties bij patiënten die stamcel- en beenmergtransplantaties ondergaan en ter
- Melk en melkproducten en voeding met een hoge glycemische index - westers dieet - spelen grote rol in de vorming van acne en staan aan de basis van veel immuunziektes als diabetes 2 en ook kanker
- Methylglyoxal, een overzicht van bekende studies en artikelen met methylglyoxal
- Mond- en keelkanker: wie voor een operatie in het hoofd- halsgebied speciale immuunversterkende voeding (arginine, RNA) krijgt heeft significant minder last van complicaties zoals infecties na de operatie en geneest sneller
- Moxibustion - verwarmingstechniek bij acupunctuur naast chemo en - of bestraling vermindert significant bijwerkingen en vergroot 5 jaars overleving bij neuskeelkankerpatiënten van 35,7% naar 50% blijkt uit kleinschalige maar wel gerandomiseerde studie
- NADH: Wat is het middel NADH en werkt dat echt tegen vermoeidheidverschijnselen en bij hormoonbehandelingen bij o.a. borstkanker als ondersteuning?
- Noni, een vruchtendrankje met immuunversterkende kwaliteiten
- Opereren van longkanker patiënten in de zomer geeft significant betere resultaten, minder recidieven, dan opereren in de winter of voorjaar. Vitamine D. lijkt hierin een grote rol te spelen.
- Orgotein - Super Oxyde Dismutase (SOD) verbetert hoog significant de bijwerkingen die optreden bij bestraling van hoofd- en halsgebied waar kanker optrad
- Paardenmelk lijkt goed voor de gezondheid..
- Pancreasenzym (alvleesklierenzym) met ondersteuning van dieet en suppletie geeft zeer opmerkelijke en hoopvolle resultaten in onderzoek van Dr. Gonzalez en Dr. Linda Lee Isaacs
- Panceasenzymtherapie geeft opmerkelijk goede resultaten bij dierproeven met alvleesklierkanker. en bevestigt aanpak van Dr. Gonzalez.
- PC-SPES en Prostasol - Mix van Chinese kruiden bij prostaatkanker geeft een bijzonder positief effect op kwaliteit van leven en veel langere levensduur. Zie alle informatie over PC-SPES/Prostasol bij elkaar gebracht op 1 pagina
- Probiotica melkzuurbacteriëen: een overzicht van studies en artikelen over toepassing van probiotica naast behandelingen van kanker en herstel van darmflora na belastende behandelingen
- PSK en PSP de medicinale paddestoelen die een grote antioxidante werking hebben. Een overzicht van belangrijke studies en artikelen.
- Q-10: Het natuurlijke niveau van Q-10 in het bloed van melanoompatiënten lijkt een onafhankelijke en betrouwbare voorspeller voor de kans op het krijgen van wel of geen recidief blijkt uit een gerandomiseerde studie met totaal 220 deelnemers
- REOLYSIN: Virusinjectie (REOLYSIN) geeft in fase I studie veelbelovende resultaten bij kankerpatiënten met solide tumoren, waaronder hersentumoren en prostaatkanker
- Orgotein - Super Oxyde Dismutase (SOD) geeft hoog significante bescherming tegen ernstige bijwerkingen van bestralingen in het bekken- en buikgebied, aldus gerandomiseerde studie bij 100 patiënten met rectumkanker
- Resveratrol - een stofje met anti kanker werking staat ter discussie door fraude van 1 wetenschapper, maar overzichtstudie toont aan dat resveratrol wel degelijk anti kanker eigenschappen heeft
- Selenium studie referenties - 66 in totaal - bij elkaar gezet als bewijs van preventieve en therapeutische rol van selenium.
- St Janskruid als aanvullend middel bij kanker
- Sulphuraphane - Sulfurofaan een stofje vooral voorkomend in broccoli bewijst opnieuw effectieve en veilige behandeling van kanker te kunnen zijn, nu bij prostaatkanker en borstkanker.
- Traumeel S. een homeopatisch middel voorkomt stomatitis bij kinderen die een beenmergtransplantatie of stamceltransplantatie ondergaan, blijkt uit dubbelblinde gerandomiseerde studie.
- Theophylline, een middeltje verwant aan caffeïne beperkt significant bijwerkingen van op cisplatin gebaseerde chemokuren en beschermt de nieren tijdens chemokuren bij patiënten met verschillende kankersoorten
- Total Parental Nutrition - TPN - voeding via bloedbaan - met 50 - 50 of 80 - 20 verhouding van glucose/vet is bewezen slechter dan normale orale bijvoeding (EN) als bijvoeding van verzwakte kankerpatienten
- Ukrain al of niet in combinatie met Gemzar - gemcitabine zorgt voor verdubbeling van overlevingstijd bij inoperabele alvleesklierkankerpatiënten, aldus gerandomiseerde fase II studie met 90 patiënten.
- Ureumzalf voorkomt significant hand-voet syndroom - pijnlijke handen en voeten - in vergelijking met vette zalf zonder ureum
- Visolie - Omega 3 vetzuren: enkele artikelen en informatie over waarde van Omega vetzuren bij elkaar gezet
- Wasabi: Heeft natuurlijke wasabi, een smaakversterkende saus gemaakt uit de wortel van de wasabiplant, ook medicinale kwaliteiten tot aan remming van kanker aan toe?
- Waterstoftherapie bewijst meer en meer waarde bij chronische ziektes en ook bij vormen van kanker bewijzen studies dat kankerpatienten profijt kunnen hebben van waterstofbehandelingen
- Yoga verbetert slaap en kwaliteit van leven bij overlevenden van kanker met slapeloosheid. Blijkt uit grote fase III studie



Plaats een reactie ...
1 Reactie op "Capsaicin zalf uitwendig aangebracht, vermindert significant neurologische pijn (zenuwpijnen) veroorzaakt door operatieve ingrepen bij kankerpatiënten maar chilipepers met veel capsaicin werken ook goed als pijnstiller."